Medicare: Spending on Certain Disposable Wound Care Devices in Home Health
Fast Facts
Medicare covers “durable” medical devices, but disposable devices—which are used one time—are generally not covered.
Since 2017, Medicare has covered disposable negative pressure wound therapy devices that home health agencies provide to homebound beneficiaries. The devices apply airtight pressure to cover wounds, such as diabetic ulcers, and suction away fluid to promote healing.
We found that Medicare paid home health agencies about $735,000 for these devices, provided to 340 beneficiaries from January 2017–June 2018.
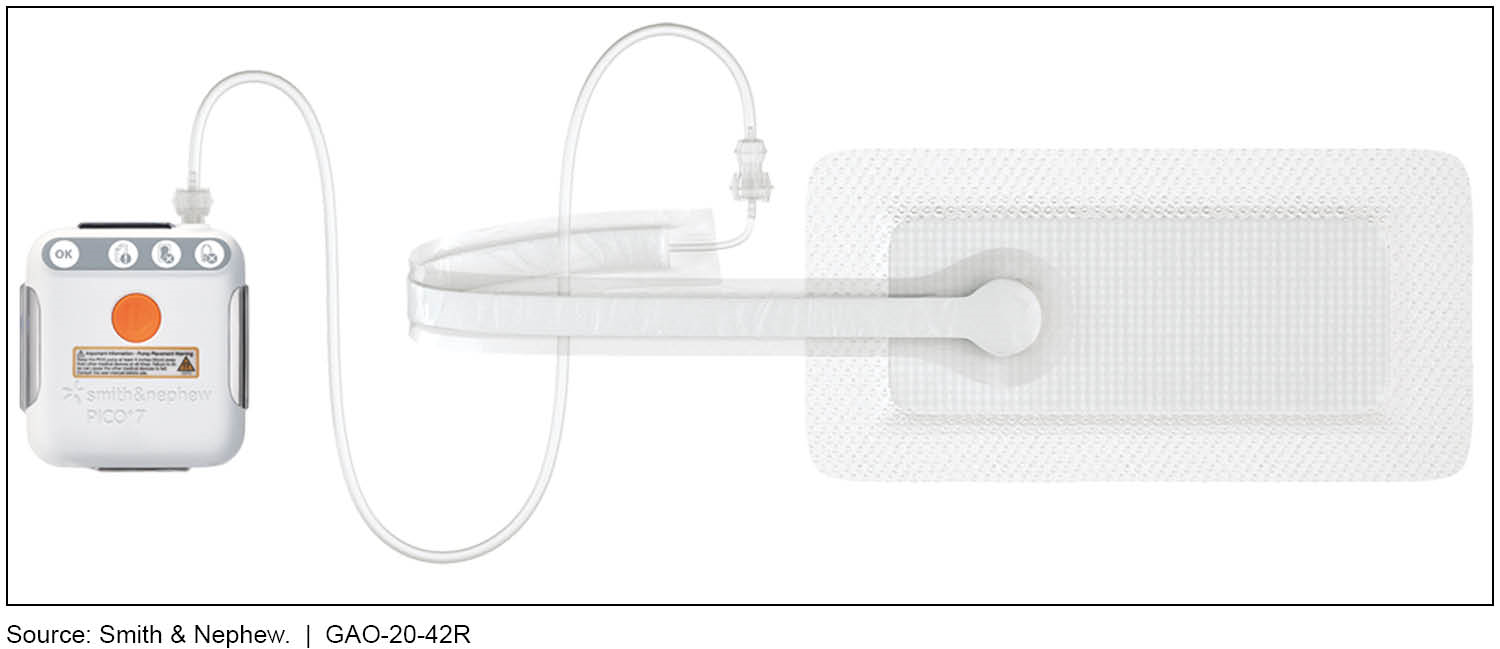
Example of a Disposable Negative Pressure Wound Therapy Device

Medical device
Highlights
What GAO Found
The Consolidated Appropriations Act, 2016, provided for a separate payment to Medicare home health agencies for the furnishing of disposable negative pressure wound therapy (NPWT) devices as of January 1, 2017. NPWT devices covered under Medicare’s home health benefit are used to treat a number of specific conditions, including pressure and diabetic ulcers, and certain wounds initially treated in an inpatient setting. NPWT devices involve the application of an airtight dressing on the wound, which is then connected through tubing to a NPWT device that applies negative pressure, or suction, to remove fluid and debris from the wound to promote healing. Disposable NPWT devices are designed for single use over a period of days or weeks, and more than one disposable device may be needed during the course of wound healing treatment (see figure).
Figure: Example of a Disposable Negative Pressure Wound Therapy Device
From January 1, 2017 to June 30, 2018, Medicare covered 3,978 disposable NPWT devices furnished by home health agencies, with spending, including beneficiary coinsurance, totaling $923,340. Of this total amount, Medicare paid $735,490, and the average payment per furnished device was $185. Medicare beneficiaries are responsible for a 20 percent coinsurance payment for disposable NPWT devices. The average total coinsurance amount beneficiaries paid for the disposable NPWT devices they received was $553, with an average payment amount of $47 per furnished device.
Outside of Medicare, GAO found limited coverage for disposable NPWT devices for use in the home, based on its review of publicly available medical policies and coverage information. For the five selected state Medicaid programs that GAO reviewed, the publicly available information we reviewed did not explicitly establish coverage for disposable NPWT devices. Most of the eight commercial insurers GAO reviewed do not currently cover home use of disposable NPWT devices.
We provided a draft of this correspondence to the Department of Health and Human Services for review and comment, and it did not have any comments.
Why GAO Did This Study
Medicare covers durable medical equipment (DME) that can be used in the home and has an expected lifetime of at least 3 years, among other criteria. Disposable devices are generally not covered by Medicare for use in the home because they are not considered durable, with the exception of disposable NPWT devices, which are covered under Medicare’s home health benefit.
The Consolidated Appropriations Act, 2016, included a provision for GAO to report to Congress on the effect of paying for disposable NPWT devices under the Medicare home health benefit and provide information on state Medicaid agency and commercial insurer coverage of disposable NPWT devices. This report describes Medicare home health utilization and spending for disposable NPWT devices, and other payer coverage of disposable NPWT devices. GAO analyzed Medicare home health claims data for the period of January 1, 2017 through June 30, 2018—the most recent data at the time of our review; interviewed Centers for Medicare & Medicaid Services officials and stakeholders, including home health and DME associations and device manufacturers; and reviewed publicly available medical policies and coverage information for five state Medicaid programs and eight commercial insurers. GAO selected the state Medicaid programs and commercial insurers based on high beneficiary enrollment, as well as information on disposable NPWT coverage provided by stakeholders.
For more information, contact Jessica Farb at (202) 512-7114 or farbj@gao.gov.
