Medicaid: Enrollment in and CMS Oversight of Former Foster Care Children Eligibility Group
Fast Facts
Nearly all children in foster care are eligible for Medicaid. After they age out of foster care, usually at 18, most remain eligible for coverage until 26. Over 100,000 of these young people had Medicaid in 2023.
But it's hard for some young people to maintain their coverage. For example, some may miss communications because they change addresses frequently. Others may avoid seeking help because they don't trust state agencies.
To reach them and ensure they get the coverage they're entitled to, some states collaborate with trusted organizations that supported them while they were in foster care. Other states use text messages to reach them.

Highlights
What GAO Found
Medicaid is a joint state-federal health care financing program for certain low-income and medically needy individuals. The program covers certain individuals who aged out of foster care, ages 18 to 26, through the Former Foster Care Children eligibility group, regardless of their income. At least 112,000 individuals were enrolled in this group during 2023, according to GAO analysis of Medicaid data. These individuals comprised less than 1 percent of Medicaid beneficiaries.
Number of Individuals Enrolled in the Former Foster Care Children Medicaid Eligibility Group in 2023
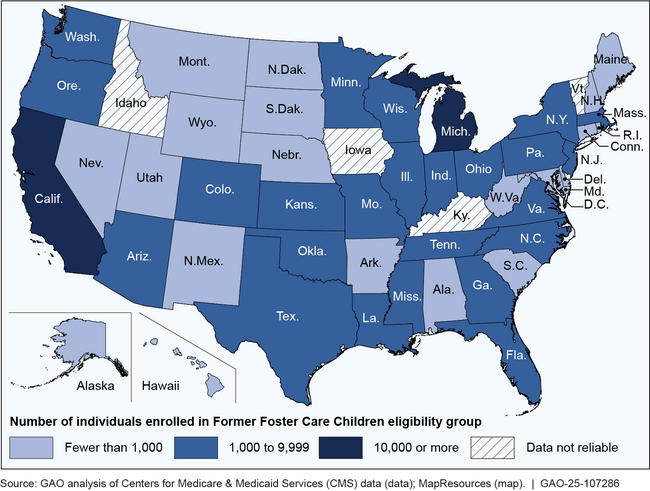
Note: For more details, see figure 2 in GAO-25-107286.
Individuals who have aged out of foster care can face barriers to enrolling in Medicaid and maintaining coverage. For example, they may miss Medicaid outreach if they change addresses frequently due to unstable housing, or avoid seeking assistance due to mistrust of state agencies, according to officials in selected states and the Centers for Medicare & Medicaid Services (CMS), which oversees Medicaid. States' approaches to address these barriers include using text messaging to reach individuals and collaborating with trusted organizations that have supported individuals in foster care.
CMS provided guidance to states on enrolling individuals formerly in foster care in Medicaid, and conducted general monitoring of Medicaid eligibility, which includes the Former Foster Care Children eligibility group.
Why GAO Did This Study
Individuals who experience foster care are more likely to have complex health needs as compared with the general population, according to CMS. Over the past decade, Congress has established and expanded Medicaid coverage options for individuals formerly in foster care that meet certain criteria.
GAO was asked to provide information about efforts to enroll individuals formerly in foster care into Medicaid. Among other things, this report addresses the size of the Former Foster Care Children eligibility group; barriers this population faces enrolling in Medicaid, and selected states' approaches to addressing them; and CMS oversight of enrollment in the Former Foster Care Children eligibility group.
GAO analyzed reliable 2023 Medicaid eligibility and age data from 46 states and the District of Columbia. GAO also analyzed CMS and selected states' documents; and interviewed officials from CMS, selected states' Medicaid and child welfare agencies, and organizations that work with individuals formerly in foster care or on issues related to aging out of foster care and Medicaid. GAO selected these states—Arizona, California, Georgia, Indiana, Massachusetts, New York, North Carolina, and Ohio—based on factors such as variation in the number of individuals in foster care and geography. GAO also conducted a site visit to Georgia.
For more information, contact Jessica Farb at (202) 512-7114 or FarbJ@gao.gov.
