Medicare: Performance-Based and Geographic Adjustments to Physician Payments
Fast Facts
For decades, Congress and Medicare have worked on improving how Medicare pays health care providers to incentivize high quality, efficient care for beneficiaries.
In this testimony, we discussed our prior work on Medicare's Quality Payment Program, which includes:
The Merit-based Incentive Payment System, which adjusts Medicare payments based on factors like cost and quality of care
The Advanced alternative payment model, in which payments can increase if a provider meets care quality goals, but payments could decrease for falling short
Providers' experiences with these systems revealed both benefits and challenges.

Highlights
What GAO Found
To implement the Quality Payment Program in 2017, the Centers for Medicare & Medicaid Services (CMS) established two tracks to financially incentivize Medicare providers to deliver high quality, efficient care:
--The Merit-based Incentive Payment System (MIPS) allows eligible providers to earn performance-based payment adjustments.
--The Advanced Alternative Payment Model (Advanced APM) encourages providers to share in the financial rewards and risk of caring for beneficiaries.
Most physicians providing Medicare services must participate in one of the two tracks.
In October 2021, GAO reported that from 2017 through 2019, at least 93 percent of providers under MIPS earned a positive adjustment while less than 5 percent qualified for a negative adjustment. The highest amount of positive adjustment was 1.88 percent.
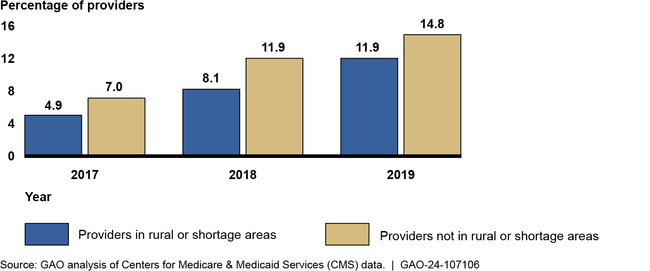
In November 2021, GAO reported that the proportion of eligible providers who participated in Advanced APMs was lower among providers in rural or shortage areas compared to other areas in each year from 2017 through 2019. (See figure.) Most providers who participated were eligible to earn the 5 percent incentive payment, regardless of their practice area.
Percentage of Medicare Providers in Rural or Shortage Areas and Providers Not Located in These Areas Who Participated in Advanced APMs, 2017 – 2019
Medicare adjusts the amount it pays for physician services to account for differences in the costs of providing care across various geographic locations. Specifically, Medicare will pay more for a physician's service in an area where approximate costs for a physician's time, skills, and effort are higher than the national average and less in an area where costs are lower. GAO reported in 2022 that the modeling for geographic variation generally accounted for physician earnings in most localities (90 of 119 localities). However, in 14 localities, physician earnings were lower than the amount suggested by the analysis, and in 15 localities, physician earnings were higher.
Why GAO Did This Study
With Medicare enrollment and spending projected to increase, controlling program spending remains a serious long-term financial challenge. Physicians and other providers play a central role in the growth of Medicare expenditures both through the services they provide and the services they order such as diagnostic tests and referrals. In 2021, Medicare payments to approximately 1.3 million physicians and other providers were about $93 billion. This represented about 18 percent of all traditional Medicare expenditures.
For decades, Congress and CMS have worked to refine the Medicare physician fee schedule to incentivize high-quality, efficient care. For example, the Medicare Access and CHIP Reauthorization Act of 2015 authorized the Quality Payment Program.
This statement summarizes GAO's previously issued reports on (1) the Quality Payment Program and the two tracks it established to incentivize Medicare providers, and (2) geographic adjustments to physician payments.
This statement is based on GAO's October 2021 report on the MIPS, its November 2021 report on the Advanced APMs, and its February 2022 report on geographic adjustments to physician payments. Details on the objectives, scope, and methodology of this work can be found in each issued report.
For more information, contact Leslie V. Gordon at (202) 512-7114 or gordonlv@gao.gov.
