Havana Syndrome: Better Patient Communication and Monitoring of Key DOD Tasks Needed to Better Ensure Timely Treatment
Fast Facts
In 2016, U.S. Embassy staff and their families in Havana, Cuba, suddenly began having symptoms such as head pain, tinnitus, blurry vision, vertigo, and more. These symptoms, once called "Havana Syndrome," have since been reported by personnel around the world and are now called "anomalous health incidents."
Laws require DOD to treat current and former federal employees and family members diagnosed with this poorly understood condition. But many of these people have said it's hard to access care in a military health system they aren't familiar with.
We recommended DOD develop written guidance to standardize care for such patients, and more.
U.S. Embassy in Havana, Cuba

Highlights
What GAO Found
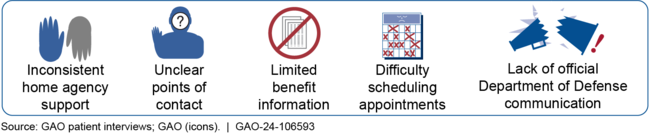
U.S. government employees and family members in several countries have experienced a sudden onset of symptoms referred to as anomalous health incidents (AHI). GAO interviewed 65 AHI patients, who reported a variety of challenges in accessing the Military Health System (MHS). They included inconsistent support from home agencies before seeking MHS treatment, limited information and unclear points of contact upon entering the MHS, and difficulty scheduling appointments when using the MHS. According to officials, civilian AHI patients are not as familiar with the MHS as active-duty military and need additional support to navigate the system. In addition, the Department of Defense (DOD) lacks an official mechanism to communicate authoritative information to AHI patients, which led some to use informal support groups to navigate the MHS. While some patients found these groups valuable, other patients and DOD officials noted these groups sometimes communicated inaccurate information. For example, some officials reported misinformation in the groups about the availability of appointments in the MHS. Without an official DOD mechanism to communicate with AHI patients, this situation can perpetuate inaccuracies, fuel perceptions of inequity, and lessen trust in MHS providers.
Challenges Reported by Anomalous Health Incident Patients Accessing the Military Health System
DOD has created a plan to address some access concerns of AHI patients, but it contains uncertain timeframes and lacks monitoring provisions. For example, the plan produced a new approval process for AHI patients to enter the MHS and calls for an enhanced AHI Care Coordination Cell to centralize administrative and clinical processes. However, the timeframe for implementing the care cell has been delayed. Moreover, the plan does not contain components for monitoring these two key tasks, which could undercut its success.
DOD has developed a registry as required by law to include certain data on AHI patients assessed or treated by DOD. However, the AHI Registry data fields remain under development. Moreover, delays in obtaining individual consent for inclusion have limited the number of patients contained in the AHI Registry. DOD did not initially seek consent from individuals to be included in the registry when they entered the MHS, limiting the number of participants. Of 334 AHI patients who had qualified for care in the MHS in January 2024, only 33 had been entered in the AHI Registry as of May 2024. According to DOD, key agencies also have not signed memorandums of agreement with DOD, which has contributed to the slow inclusion of AHI patients. Without a plan to gather consent from AHI patients who have left the MHS, DOD will have a limited number of patients in the AHI Registry to analyze, which could limit its usefulness for supporting AHI analysis and research activities.
Why GAO Did This Study
In 2016, Department of State staff at the U.S. Embassy in Havana, Cuba, began experiencing a sudden onset of symptoms, usually following a loud sound. These included head pain, tinnitus, vision problems, vertigo, and cognitive difficulties. These events, first labeled “Havana Syndrome,” are now referred to as AHIs and have affected employees (and their families) of various federal agencies overseas and domestically. Federal law requires DOD to provide treatment to U.S. government employees (current and former) and their family members diagnosed with AHI conditions or related afflictions at an appropriate military treatment facility.
GAO was asked to review DOD's efforts to facilitate AHI patients' access to the MHS and develop an AHI Registry. This report examines (1) the challenges AHI patients have faced accessing care in the MHS, (2) how DOD is facilitating AHI patients' access to the MHS, and (3) the extent to which DOD has developed a registry to facilitate AHI research. GAO reviewed DOD planning documents and interviewed officials. GAO also interviewed, both in-person and virtually, 65 AHI patients from various federal entities on their experiences accessing the MHS.
Recommendations
GAO is making six recommendations to DOD, including that DOD develop written guidance, establish a mechanism for official communication with AHI patients, implement its AHI care cell, monitor initiatives, and create a plan to gather registry consent from patients who have left the MHS. DOD concurred with the recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Defense Health Agency | The Director of DHA should develop written guidance to facilitate AHI patient understanding of the MHS, such as through the handbook proposed in the Plan of Action and Milestones. (Recommendation 1) |
DOD concurred with our recommendation, and in response, developed several guidance documents. This includes (1) a 15-page patient welcome packet on base access, treatment expectations, among other topics; (2) a one-pager explaining coverage of durable medical equipment; and (3) a one-pager that provides checklists of the necessary steps for TRICARE and Non-TRICARE patients to receive treatment for Anomalous Health Incidents from the DOD system. DOD disseminated these documents to the Intrepid Spirit Centers, which provide care to AHI patients, on January 16, 2025. Furthermore, DHA has published the two one-pagers on the AHI page of the Health.mil website. As a result of this formal, written guidance, AHI patients will receive the same information during their initial outreach, which will allow them to navigate the MHS on more equal footing, leading to more consistent levels of care.
|
| Defense Health Agency | The Director of DHA should establish a mechanism to systematically furnish official information to its AHI patients. (Recommendation 2) |
DOD concurred with our recommendation, and in response, established a central location for AHI information on its website for AHI patients. Additionally, DHA distributed materials on its website to other federal agencies. DHA also created an AHI information phone line, which is exclusively for AHI patients to connect with an AHI Care Coordinator at the National Intrepid Center of Excellence. DHA's AHI Patient Welcome Packet contains the information line contact number, and the other Intrepid Spirit Centers, which provide care to AHI patients, have also received the information line contact number. As a result of these steps, DHA has established mechanisms to systematically furnish official information to AHI patients. These mechanisms could reduce AHI patients' reliance on informal networks, which could increase trust in MHS providers' treatments and lessen perceptions of inequitable care experiences in the MHS.
|
| Defense Health Agency | The Director of DHA should fully implement the new care cell for AHI patients. (Recommendation 3) |
DOD concurred with our recommendation, and in response, took steps to fully implement the AHI Care Coordination Cell, including by developing a procedure guide to specifically support the Cell's AHI Care Coordinators and medical support assistants. This care coordination guide was distributed to the other Intrepid Spirit Centers, which provide care to AHI patients, in March 2025. Further, three nurse care managers have been hired at the National Intrepid Center of Excellence to implement the AHI Care Coordination Cell, according to the guide's outlines. By developing these procedures and hiring new staff to implement them, DHA has fully implemented its AHI Care Coordination Cell. As a result, DHA is better positioned to increase the administrative support that AHI patients receive, which would reduce scheduling problems and delayed access to care.
|
| Defense Health Agency | The Director of DHA should add a monitoring component to the Plan of Action and Milestones on the new AHI entry process' timing. (Recommendation 4) |
DOD concurred with our recommendation, and in response, DHA utilized its Enterprise Task Management Software Solution (ETMS2) for monitoring new patient approvals for care in the MHS. DHA provided an example of the information displayed for a patient approval. ETSM2 shows DHA which component or components of DHA have been assigned a task for the patient approval. Further, the system displays the date the component was assigned a task, the date the task is due, and the actual completion date. According to DOD officials, DHA uses information from this system in bi-weekly interagency meetings, where it provides updates on new patients entering the MHS system, discusses approval process delays, and engage in real-time mitigation strategies. As a result of this monitoring system, DHA is verifying it is meeting its 10-business day deadline to approve patients, in addition to identifying and addressing any systematic delays in the approval process. Addressing these delays can promote better health outcomes for AHI patients by reducing the amount of time to approve evaluation and treatment of their symptoms.
|
| Defense Health Agency | The Director of DHA should add a monitoring component to the Plan of Action and Milestones on the performance of the new care cell for AHI patients. (Recommendation 5) |
DOD concurred with our recommendation, and in response, developed several mechanisms to gather information on the performance of the AHI Care Coordination Cell. First, DHA deployed an outpatient experience questionnaire to collect patient feedback on their AHI care in the military health system. Second, DHA developed two trackers: one to capture the number of calls made to the National Intrepid Center of Excellence, and another to monitor the number of AHI patients, and their current treatment status in the military health system. As a result of these steps, DHA has added a monitoring component for its AHI Care Coordination Cell. By monitoring the AHI Care Coordination Cell, DHA may ensure that the cell is offering additional administrative support and standardized care experiences to AHI patients, which could reduce the challenges AHI patients reported in using the MHS.
|
| Defense Health Agency | The Director of DHA should develop a plan to gather AHI Trauma Registry consent from individuals who have finished their care in the MHS. (Recommendation 6) |
DOD concurred with our recommendation, and in response, DHA created instructions for providers on how to gather consent from patients who had completed their care in the MHS. DHA disseminated the instructions to the Intrepid Spirit Centers, which care for AHI patients, in January 2025. In addition, DHA added the instructions to the AHI page of their health.mil website under "provider resources." As a result of these updated instructions, DHA is standardizing its process for gathering consent from AHI patients who have completed their care in the MHS. Standardizing this process could allow DHA to add more patients to its AHI trauma registry, which would expand the available information in, and ensure the eventual usefulness of, the registry.
|
