Medicaid Managed Care: Rapid Spending Growth in State Directed Payments Needs Enhanced Oversight and Transparency
Fast Facts
States and the federal government pay managed care plans based on the number of Medicaid beneficiaries. The managed care plans then pay health care providers for services. Since 2017, states have been allowed to steer additional payments to providers to help the state achieve certain Medicaid goals.
State directed payments should have been exceptions to the regular payment process, but they now comprise a significant and growing proportion of managed care spending.
States find the strategy useful, but are these payments achieving intended goals? We recommended better oversight, evaluation, and more to ensure that these payments are effective.

Highlights
What GAO Found
Using state directed payments, states can direct how Medicaid managed care plans pay providers in certain circumstances. This includes requiring payments in addition to the base payment rates negotiated between plans and providers. State directed payment spending has grown to at least $38.5 billion in 2022, the sixth year of state use, and further growth is expected.
Estimated 2022 Spending for State Directed Payments, by State
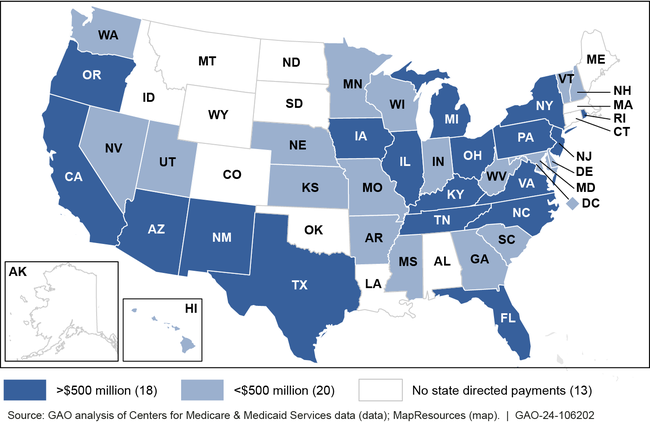
Note: For more details, see figure 3 in GAO-24-106202.
States often relied on taxes on providers, instead of state general funds, to finance the nonfederal share of state directed payments. States' limited stake in the cost of state directed payments raises concerns for GAO given the weaknesses GAO identified in the Centers for Medicare & Medicaid Services' (CMS) policies and procedures for approving such payments.
- Weak fiscal guardrails. CMS has indicated that payments must be reasonable and appropriate, but has not established and communicated a definition of, or standards for, assessing that. CMS has set no other limits on spending under directed payments.
- No consideration of payment outcomes when renewing. CMS does not appear to consider state evaluation results or any other outcome information when deciding whether to approve a renewal of a directed payment.
- Gaps in transparency. CMS recently made payment applications publicly available, but does not post other information, such as attachments including important financing information, evaluation plans, and evaluation results.
These weaknesses leave the agency at risk of approving ineffective payments.
Why GAO Did This Study
In 2022, spending for managed care represented more than half of the $800 billion spent on Medicaid. The percentage is expected to continue growing in the next decade. With few exceptions, states may not direct managed care plans' payments to providers. However, CMS began allowing a new exception in 2017: state directed payments. Since then, states have made widespread use of directed payments; for example, to increase payments to safety net providers to ensure beneficiary access.
Among other issues, this report describes estimated spending for, and state financing of, state directed payments, and examines CMS's policies and procedures for approving these payments.
GAO analyzed information on approved state directed payments in effect in 2022, and interviewed CMS and Medicaid officials from five states. These states were selected, in part, based on having a directed payment estimated at $1 billion or more in 2022. GAO assessed CMS's policies and procedures against agency guidance and federal internal controls.
Recommendations
GAO is making four recommendations to CMS, including to enhance the agency's fiscal guardrails for approving state directed payments, review outcome information at renewal, and make publicly available additional approval documents. The Department of Health and Human Services agreed with two recommendations. It neither agreed nor disagreed with the other two recommendations, but noted CMS actions underway to address them.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services |
Priority Rec.
The Administrator of CMS should enhance the agency's fiscal guardrails for approving state directed payments by establishing a definition of, and standards for, assessing whether directed payments result in payment rates that are reasonable and appropriate, and communicating those to states; determining whether additional limits are needed; and requiring states to submit data on actual spending amounts at renewal. (Recommendation 1) |
HHS neither agreed nor disagreed with this recommendation but highlighted that provisions in a May 2023 CMS proposed rule should address the recommendation. In May 2024, CMS finalized the rule, which included activities that enhance the agency's fiscal guardrails for state directed payments. For example, the final rule requires states to submit data to CMS on the total dollars expended by each managed care organization for state directed payments paid to providers. As of August 2024, CMS officials also indicated that the agency would be revising review procedures to reflect the need to consider any available spending data when approving a renewal of a state directed payment and noted that the agency plans to issue related technical guidance. In July 2025, federal law was enacted directing CMS to reduce the total payment rate for state directed payments for certain provider types beginning on or after July 4, 2025, which in effect creates a standard for what is reasonable and appropriate for those payments. In February 2026, CMS issued preliminary guidance while the agency prepares proposed rulemaking. When CMS completes revision of its review procedures, issues the technical guidance, and promulgates the new rules, we will reassess this recommendation for closure.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should consider interim evaluation results or other performance information from states at renewal to gain more timely information on whether state directed payments are advancing quality goals. (Recommendation 2) |
In May 2024, CMS finalized a rule that includes a new requirement that state directed payments must result in the state achieving the goals and objectives of the payments and states must submit evaluation results to CMS upon request. The rule also details what must be included in state directed payment evaluation plans and requires states to submit evaluation reports for certain large/ high-dollar state directed payments--those where the estimated cost of the payments exceeds 1.5 percent of the state's total Medicaid spending. According to CMS officials, these new requirements provide CMS with the authority to consider additional evaluation results at renewal and disapprove state directed payment renewals that do not meet the state's goals and objectives of the payments. The addition of these evaluation requirements will allow CMS to gain more timely information on whether state directed payments are advancing quality goals to consider at renewal.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should require states to consider health equity priorities in designing evaluations of state directed payments. (Recommendation 3) |
At the time the report was issued, HHS agreed with this recommendation and noted additional rulemaking may be necessary to implement this recommendation. In June 2024, CMS noted that final rules issued in August 2023 require stratification of certain quality measures by age, race, and other demographics. These requirements will be phased in over the next 5 years. CMS indicated that as stratification becomes more prevalent, the agency will encourage more state evaluation of differences in outcomes across demographic characteristics. In February 2025, CMS notified GAO that the agency no longer concurs with the recommendation and replaced its prior Health Equity Framework with the Framework for Healthy Communities. The new framework includes priorities similar to the previous framework, such as gathering better data to close gaps in health outcomes and drive quality improvement. CMS has not required states to incorporate its framework priorities into state directed payment evaluations. In September 2025, CMS issued an Informational Bulletin outlining the requirements for State Directed Payment evaluations. The Informational Bulletin does not include any requirements for states to consider health equity or health disparity priorities in designing evaluations of state directed payments. As such, state evaluations will continue to lack information that would allow states and CMS to assess differences in outcomes by population, which is necessary for improving quality of care.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should make publicly available all approval documents related to new and renewed state directed payments, including application attachments, state evaluation plans, and evaluation results. (Recommendation 4) |
HHS agreed with this recommendation. In August 2024, CMS officials told us that the agency is planning to post all approved state directed payment documents on its website but has had to delay those efforts given other priorities. Officials indicated that the agency is also working on changes to the state directed payment application that will allow the agency to capture more information in an accessible format and reduce the need for attachments that are complex to convert to an accessible format. As of February 2025, GAO continues to monitor CMS progress toward implementing this recommendation and will reconsider closure when CMS releases the updated application template.
|
