COVID-19 Provider Relief Fund: HRSA Continues to Recover Remaining Payments Due from Providers
Fast Facts
The Provider Relief Fund spent $135 billion to help health care providers with COVID-related expenses and lost revenue during the pandemic. Most of the relief payments—about $85 billion—went to hospital-based health systems and hospital-affiliated providers.
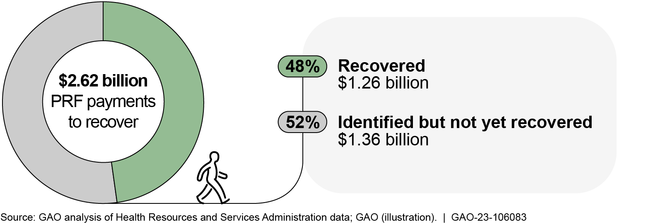
To confirm that payments were accurate, the Health Resources and Services Administration took steps to review provider eligibility and if funds were used appropriately. In doing so, it found that $2.6 billion in payments should be recovered.
As of May 2023, the agency had recovered about half of the money and, as of August 2023, had set a schedule to get back the rest.

Highlights
What GAO Found
The Health Resources and Services Administration (HRSA), an agency within the Department of Health and Human Services (HHS), administers and oversees the Provider Relief Fund (PRF). The PRF provided relief to health care providers for expenses or lost revenues attributable to the COVID-19 pandemic. As of May 2023, HRSA distributed $135 billion in payments kept by providers; hospital-based health systems and hospital-affiliated providers received the majority of payments—about $84 billion. HRSA made payments until June 2023, when the remaining unobligated funds for provider relief payments were rescinded.
Among its efforts to ensure payment accuracy, HRSA conducted pre-payment reviews to verify provider eligibility and information on provider applications. HRSA also conducted post-payment reviews to check for potential payment errors and identify overpayments. HRSA plans to conduct these reviews on 59 types of potential payment errors, but the agency has been delayed in completing these reviews. As of May 2023, 21 of 59 remained open. In October 2021, GAO recommended that HRSA promptly complete the remaining reviews, but HRSA has not yet implemented the recommendation.
HRSA has taken steps to ensure that providers used PRF payments according to program requirements. HRSA required providers to report on their use of PRF payments, and it has been auditing a risk-based sample of providers to verify appropriate use of payments. HRSA also assessed fraud risks and implemented controls to ensure proper use of payments, though certain processes were only recently implemented. In particular, HRSA implemented recommendations from its 2021 fraud risk assessment. In March 2023, HRSA implemented a process to review irregular payments and, in June 2023, finalized procedures for responding to potential fraud.
As of May 2023, HRSA had recovered about half of the $2.62 billion in payments identified for recovery. HRSA had established time frames to recover most of the $1.36 billion in payments not yet recovered, but had not established time frames to recover $250 million in remaining overpayments, unused payments, and some payments from non-compliant providers. However, in August 2023, HRSA established time frames for the recovery of these payments.
Provider Relief Fund (PRF) Payment Recoveries, as of May 2023
Why GAO Did This Study
The PRF was created in March 2020 to provide COVID-19 relief to health care providers and ensure access to essential health care services. Providers included those enrolled in Medicare, Medicaid, and the Children's Health Insurance Program.
The CARES Act includes a provision for GAO to monitor and report on the federal response to the COVID-19 pandemic. This report describes (1) PRF payment distributions; and examines (2) efforts to ensure the accuracy of PRF payments, (3) efforts to ensure that PRF payments were used according to program requirements, and (4) the status of efforts to recover PRF payments.
GAO analyzed data on PRF payments as of December 2022, by which time nearly all PRF payments had been distributed. GAO analyzed recoveries of PRF payments as of May 2023—the most recent data available at the time of the review. GAO also reviewed information and agency documentation on payment integrity activities, including program reports and risk assessments; interviewed agency officials; and compared payment integrity activities to agency requirements.
GAO's draft report recommended that HRSA establish time frames to promptly recover remaining overpayments, unused payments and payments from all noncompliant providers. In response to the draft report, in August 2023, HRSA provided a time frame for the recovery of these payments. As a result, GAO removed the recommendation and modified the report accordingly.
For more information, contact Leslie V. Gordon at (202) 512-7114 or gordonlv@gao.gov.
