Medicaid: CMS Should Assess Effect of Increased Telehealth Use on Beneficiaries' Quality of Care
Fast Facts
Telehealth has helped people get the health care they need while reducing their COVID-19 exposure risk. At the start of the pandemic, Medicaid data from 5 states showed exponential increases in
- the number and percentage of services delivered via telehealth
- the number of Medicaid beneficiaries receiving telehealth
For example, from March 2020-February 2021, 32.5 million services were delivered via telehealth vs. 2.1 million services the prior year.
But, Medicaid hasn't collected or assessed data on the quality of care beneficiaries received from telehealth services. We recommended doing so.

Highlights
What GAO Found
GAO's analysis of Centers for Medicare & Medicaid Services (CMS) data in five selected states shows that the number and percentage of services delivered via telehealth and Medicaid beneficiaries receiving them increased exponentially at the beginning of the COVID-19 pandemic in March 2020. From March 2020 through February 2021, 32.5 million services were delivered via telehealth to about 4.9 million beneficiaries in the five states, compared with 2.1 million services to about 455,000 beneficiaries in the 12 months prior to the pandemic.
Percentage of Medicaid Beneficiaries Receiving at Least One of Their Services via Telehealth, March 2019 through February 2020 and March 2020 through February 2021
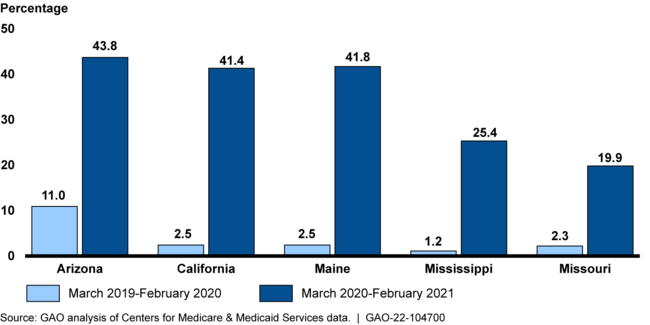
Note: GAO determined Tennessee's data were not sufficiently reliable for purposes of this analysis.
Medicaid officials from all six selected states said expanding telehealth supported beneficiaries' access to care, but also identified some limitations. Officials reported making or considering post-pandemic telehealth modifications.
CMS does not collect, assess, or report information about any effect delivering services via telehealth has on the quality of care Medicaid beneficiaries receive and has no plans to do so. Doing so is important, given concerns GAO has raised about the quality of care provided via telehealth. It would also be consistent with how CMS has encouraged states to use data on quality of care to identify disparities in health care and target opportunities for improvement to advance health equity. These efforts could begin with data for quality measures CMS already collects or through other means.
CMS neither agreed nor disagreed with GAO's recommendations. GAO maintains it is crucial for CMS to collect and analyze information to assess telehealth's effect on the quality of care Medicaid beneficiaries receive.
Why GAO Did This Study
To respond to the COVID-19 pandemic, states have expanded their coverage of telehealth in Medicaid, a jointly financed federal-state health care program for low-income and medically needy individuals.
The CARES Act includes a provision for GAO to report on the federal response to the pandemic. In addition, GAO was asked to examine the use of Medicaid flexibilities in response to COVID-19. This report describes selected states' telehealth use before and during the pandemic, and experiences with and plans for telehealth. It also evaluates, among other things, CMS's telehealth oversight of quality of services.
GAO analyzed state-reported data on telehealth use in six states selected, in part, based on variation in geography, Medicaid program size, and percentage of population living in rural areas. GAO reviewed federal oversight documents, interviewed state and federal Medicaid officials, and assessed CMS oversight against CMS guidance on using data to identify disparities in health care and target improvements.
Recommendations
GAO is making two recommendations to CMS to (1) collect and analyze information about the effect delivering services via telehealth has on the quality of care Medicaid beneficiaries receive, and (2) determine any next steps based on the results of the analysis.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should collect and analyze the information needed to assess the effect delivering services via telehealth has on the quality of care Medicaid beneficiaries receive. (Recommendation 1) |
Steps have been taken to collect and analyze the information needed to assess the effect of delivering services via telehealth, as GAO recommended. CMS officials said they continue to use tools to identify Medicaid program integrity risks associated with providing services via telehealth and to conduct data analysis to ensure that Medicaid beneficiaries are receiving appropriate services. CMS also referred us to a January 2023 study the Agency for Healthcare Research and Quality performed on the use of telehealth during the COVID-19 pandemic. The Agency for Healthcare Research and Quality determined differences in clinical outcomes were generally small and not clinically meaningful when comparing in-person services with those delivered via telehealth. CMS's ongoing efforts and the Agency for Healthcare Research and Quality's study should help ensure there are no disparities in quality of care for those who receive services via telehealth.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should determine, based on the results of its initial assessment, whether further assessments of the effect delivering services via telehealth has on the quality of care Medicaid beneficiaries receive are warranted, for the purposes of developing guidance to assist states in making telehealth coverage and payment decisions. (Recommendation 2) |
CMS has developed revised guidance to assist states in making telehealth coverage and payment decisions. Specifically, CMS issued a revised telehealth toolkit as of February 2024. The toolkit identified promising evidence of the positive effects telehealth has had on certain beneficiaries' health conditions and noted that additional evidence was still being collected regarding access to care, quality, and costs when services are delivered using telehealth. CMS noted the importance of measuring and properly understanding the effects of telehealth on quality. The toolkit includes state best practices for delivering certain services via telehealth and evaluation strategies to understand how telehealth affects quality, outcomes, and cost.
|
