Medicare: Provider Performance and Experiences Under the Merit-Based Incentive Payment System
Fast Facts
Under Medicare’s Merit-based Incentive Payment System, doctors and other providers may receive increases or decreases to their Medicare payments based on factors like the cost and quality of care they provide. We found that, from 2017-2019, over 90% of providers earned a small increase (less than 2%) to their Medicare payments.
Providers we interviewed noted some strengths and challenges of the incentive payment system. For example, some said certain design aspects of the system helped smaller practices participate, while others said they weren’t sure if it helped improve the quality of care.

Highlights
What GAO Found
The Centers for Medicare & Medicaid Services (CMS) administers the Merit-based Incentive Payment System (MIPS) under the Medicare program. Under this system, MIPS-eligible providers receive a “final score” based on their performance on certain measures in four categories, such as quality and cost of care. This final score is compared to a performance threshold and is used to determine if providers receive a negative, neutral, or positive payment adjustment applied to future Medicare payments. Providers may receive a larger positive adjustment if their final score surpasses a higher threshold, known as the exceptional performance threshold. In addition, eligible providers who do not submit required performance data may receive a negative adjustment.
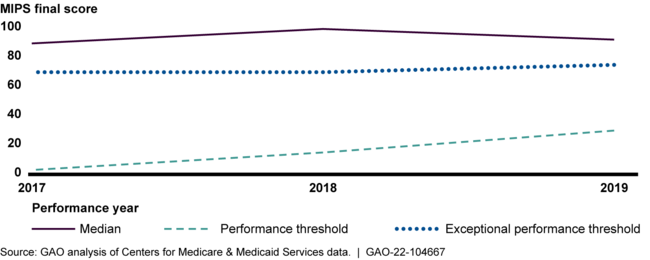
Analysis of CMS data shows that final scores were generally high and at least 93 percent of providers earned a small positive adjustment in 2017 through 2019, with the largest payment adjustment in any year being 1.88 percent. Median final scores were well above the performance threshold across each of the 3 years (see figure). About 72 to 84 percent of providers earned an exceptional performance bonus, depending on the year.
Median Final Scores Relative to Performance and Exceptional Performance Thresholds, Performance Years 2017 through 2019
Stakeholders GAO interviewed identified some strengths and challenges related to the MIPS program. For example, two of the 11 stakeholders stated that bonus points, such as those that may be added to the final scores for small practices, helped increase scores for certain providers who might otherwise be disadvantaged. Eight stakeholders questioned whether the program helps to meaningfully improve quality of care or patient health outcomes. For example, they said that the design of the program may incentivize reporting over quality improvement, with providers choosing to report on quality measures on which they are performing well, rather than on measures in areas where they may need improvement. According to CMS, the MIPS Value Pathways (MVP)—a new way of meeting reporting requirements in 2023—will help to address some of these challenges by standardizing performance measurement across specific specialties, medical conditions, or episodes of care. The development of clinically cohesive sets of measures and activities should minimize providers' selection burden in choosing measures and activities to report for each MVP, officials said.
Why GAO Did This Study
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) changed how Medicare pays for physician services, moving from a payment system that largely rewarded volume and complexity of health care services to the Quality Payment Program, which is a payment incentive program intended to reward high-quality, efficient care. Providers participate in the Quality Payment Program through one of two tracks: MIPS or advanced alternative payment models. MIPS was designed to incentivize high-quality care through performance-based payment adjustments. About 950,000 providers (about half of all Medicare Part B providers) were eligible to participate in MIPS in 2019.
Congress included a provision in MACRA for GAO to examine the MIPS program. This report describes (1) the distribution of MIPS performance scores and related payment adjustments, and (2) stakeholders' perspectives on the strengths and challenges of the MIPS program.
GAO analyzed MIPS data for performance years 2017 through 2019—the most recent year available at the time of GAO's analysis. GAO also interviewed officials from CMS and 11 selected professional organizations that represent MIPS-eligible providers of various specialties. GAO identified stakeholders through research and its analysis of the MIPS data.
The Department of Health and Human Services provided technical comments on a draft of this report, which GAO incorporated as appropriate.
For more information, contact Jessica Farb at (202) 512-7114 or FarbJ@gao.gov.
