Medicare Severe Wound Care: Spending Declines May Reflect Site of Care Changes; Limited Information Is Available on Quality
Fast Facts
People immobilized by a health condition may develop severe wounds, such as bed sores, that may require longer-term care.
Some patients get wound care at costly long-term care hospitals—facilities that mostly admit patients with multiple serious conditions. Medicare began paying less to these hospitals for more stable patients in FY2016. Since then, these facilities have seen fewer patients with severe wounds, while facilities with lower costs—e.g., inpatient rehabilitation facilities—have seen more.
There's not enough information to know if this affected quality of care, but Medicare spent less on severe wound care in FY2018 than in FY2016.

Highlights
What GAO Found
GAO's analysis of Department of Health and Human Services (HHS) Centers for Medicare & Medicaid Services (CMS) data show that in fiscal year 2018, 287,547 Medicare fee-for-service beneficiaries had inpatient stays that included care for severe wounds. These wounds include those where the base of the wound is covered by dead tissue or non-healing surgical wounds. About 73 percent of the inpatient stays occurred in acute care hospitals (ACH), and a smaller percentage of stays occurred in post-acute care facilities. Specifically, about 16 percent of stays were at skilled nursing facilities (SNF), and about 7 percent were at long-term care hospitals (LTCH).
CMS data show that Medicare spending on stays for severe wound care was $2.01 billion in fiscal year 2018, representing a decline of about 2 percent from fiscal year 2016, when spending was about $2.06 billion. Spending declined as a result of decreases in both the total number of these stays, as well as spending per stay, which both decreased by about 1 percent. The decrease in per stay spending was likely driven, in part, by a change in where beneficiaries received care. CMS data show fewer severe wound care stays in LTCHs, which tend to be paid higher payment rates. At the same time, more severe wound care stays were at two other types of facilities that tend to be paid lower payment rates: ACHs and inpatient rehabilitation facilities.
GAO's analysis of CMS data also show that, while the number of LTCHs that billed Medicare for severe wound care decreased by about 7 percent from fiscal years 2016 to 2018, Medicare beneficiaries continued to have access to other severe wound care providers. For example, CMS data show that most beneficiaries resided within 10 miles of an ACH or SNF that provided severe wound care in fiscal year 2018.
Figure: Percentage of Medicare Fee-for-Service Beneficiaries Residing within 10 Miles of a Health Care Facility That Provided Any Severe Wound Care, by Facility Type, Fiscal Year 2018
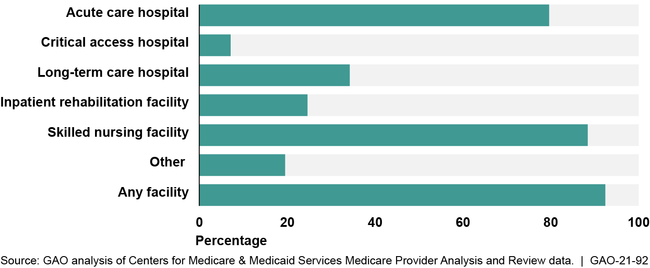
Note: The “other” category includes facilities such as psychiatric hospitals or units.
There is limited information on how or whether the decrease in LTCH care for severe wounds may have affected the quality of severe wound care Medicare beneficiaries receive. For example, CMS collects information on the percentage of patients with new or worsened pressure ulcers at post-acute care facilities, but it does not measure the quality of care they receive.
Why GAO Did This Study
Medicare beneficiaries with serious health conditions, such as strokes, are prone to developing severe wounds due to complications that often lead to immobility and prolonged pressure on the skin. These beneficiaries may require a long-term inpatient stay at an ACH or a post-acute care facility, such as an LTCH. LTCHs treat patients who require care for longer than 25 days, on average. In 2018, LTCHs represented about $4.2 billion in Medicare expenditures.
Prior to fiscal year 2016, LTCHs received a higher payment rate for treating Medicare beneficiaries than ACHs. Beginning in fiscal year 2016, a dual payment system was phased in that paid LTCHs a rate similar to ACHs for some beneficiaries and a higher rate for beneficiaries that met certain criteria. As this payment system has moved from partial to full implementation, lawmakers had questions about how it may affect beneficiaries' severe wound care.
The 21st Century Cures Act included a provision for GAO to review severe wound care provided to Medicare beneficiaries. This report describes facilities where Medicare beneficiaries received severe wound care, Medicare severe wound care spending, and what is known about the dual payment system's effect on access and quality. GAO analyzed Medicare severe wound care access and spending data for fiscal years 2016 and 2018 (the most recent data available); reviewed reports; and interviewed CMS officials, researchers, and national wound care stakeholders.
HHS provided technical comments on a draft of this report, which were incorporated as appropriate.
For more information, contact James Cosgrove at (202) 512-7114 or cosgrovej@gao.gov.
