Maternal Mortality and Morbidity: Additional Efforts Needed to Assess Program Data for Rural and Underserved Areas
Fast Facts
There's a greater risk of maternal death during pregnancy or soon after from pregnancy-related causes among rural residents, according to the Centers for Disease Control and Prevention.
CDC and the Health Resources and Services Administration fund programs aimed at reducing maternal mortality, including in rural or underserved areas where it can be harder to get health care services.
These agencies collect data—like the percentage of women receiving postpartum visits—but don't always separate and analyze this data for rural and underserved areas. We recommended they do so to help ensure program funding helps those in need.

Highlights
What GAO Found
Nationwide data from the Centers for Disease Control and Prevention's (CDC) Pregnancy Mortality Surveillance System from 2011-2016, the most recent data available at the time of GAO's review, indicate that deaths during pregnancy or up to 1 year postpartum due to pregnancy-related causes—are higher in rural areas compared to metropolitan areas. See figure. CDC data also showed higher mortality in underserved areas (areas with lower numbers of certain health care providers per capita).
Pregnancy-Related Mortality Ratios in Rural and Metropolitan Areas, 2011-2016
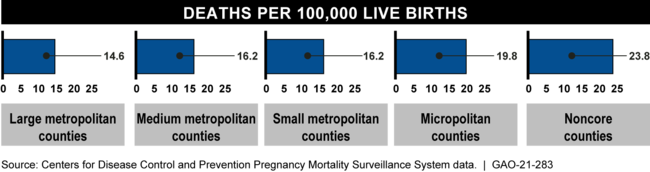
Note: Micropolitan areas include counties with populations of 2,500 to 49,999. Noncore areas include nonmetropolitan counties that do not qualify as micropolitan.
GAO also analyzed the most recent annual data available from the Agency for Healthcare Research and Quality for 2016-2018 on severe maternal morbidity (SMM)—unexpected outcomes of labor and delivery resulting in significant health consequences. Nationwide, these data showed higher estimated rates of SMM in metropolitan areas (72.6 per 10,000 delivery hospitalizations) compared to rural areas (62.9 per 10,000).
CDC and another Department of Health and Human Services (HHS) agency, the Health Resources and Services Administration (HRSA), fund several maternal health programs that aim to reduce maternal mortality and SMM, including some that target rural or underserved areas. CDC and HRSA collect program data, such as the percentage of women who received postpartum visits, to track progress in improving maternal health, but they do not systematically disaggregate and analyze program data by rural and underserved areas. By taking these actions, CDC and HRSA could help better ensure that program funding is being used to help address any needs in these areas.
HHS has taken actions to improve maternal health through its funding of various programs and releasing an action plan in 2020. HHS also has two workgroups that aim to coordinate across HHS agencies on maternal health efforts, such as program activities that aim to reduce maternal mortality and SMM. Officials from HHS's two workgroups said they coordinated in developing the action plan, but they do not have a formal relationship established to ensure ongoing coordination. Officials from one of the workgroups noted that they often have competing priorities and do not always coordinate their efforts. By more formally coordinating their efforts, HHS's workgroups may be in a better position to identify opportunities to achieve HHS's action plan goal for reducing maternal mortality and objectives that target rural and underserved areas.
Why GAO Did This Study
Each year in the United States, hundreds of women die from pregnancy-related causes, and thousands more experience SMM. Research suggests there is a greater risk of maternal mortality and SMM among rural residents and that underserved areas may lack needed health services.
GAO was asked to review maternal mortality and SMM outcomes in rural and underserved areas. This report examines, among other objectives, what is known about these outcomes; selected CDC and HRSA programs that aim to reduce these outcomes, as well as actions to collect and use relevant data; and the extent to which HHS is taking actions to improve maternal health and monitoring progress on its efforts. GAO analyzed HHS data, agency documentation, literature, and interviewed officials from a non-generalizable sample of three states and stakeholders to capture various perspectives.
Recommendations
GAO is making three recommendations, including that CDC and HRSA disaggregate and analyze program data by rural and underserved areas, and that HHS's workgroups establish a formal coordinated approach for monitoring maternal health efforts. HHS concurred with GAO's recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Disease Control and Prevention | The Director of CDC should take steps to systematically disaggregate and analyze maternal health program data by rural and underserved areas, and make adjustments to program efforts, as needed. (Recommendation 1) |
CDC concurred with this recommendation and has taken steps to implement it. As of November 2021, CDC stated that it provides ongoing technical assistance, including office hours, trainings, guidance, symposiums, and job aids, to Maternal Mortality Review Committees (MMRC) to ensure that maternal health data is appropriately analyzed and disseminated. CDC stated that this technical assistance helps to ensure that maternal health program efforts are adjusted based on available data and meet the needs of the communities that the MMRCs serve. In addition, CDC completed a variety of analyses of maternal health program data by rural and underserved areas. For example, CDC worked with Emory University to conduct an analysis of the association between pregnancy-related mortality and county-level socio-spatial indicators using geocoded Pregnancy-related Mortality Surveillance System (PMSS) data. CDC also developed a Community Vital Signs Dashboard for MMRCs, which uses geocoded data to identify how the community in which a death occurred compares to other communities, including those that are medically underserved. In August 2021, CDC released a paper on urban-rural differences in pregnancy-related deaths based on geocoded PMSS data, and stated that the agency will continue to update this analysis in the future with new data. Lastly, CDC added that within the Maternal Mortality Review Information Application (MMRIA), locations associated with each maternal death are geocoded and assigned an urban/rural designation.
|
| Health Resources and Services Administration | The Administrator of HRSA should take steps to systematically disaggregate and analyze maternal health program data by rural and underserved areas and make adjustments to program efforts, as needed. (Recommendation 2) |
HRSA concurred with this recommendation and has taken steps to implement it. As of November 2021, HRSA stated that it made program adjustments to systematically disaggregate and analyze maternal health program data by rural and underserved areas. For example, HRSA stated that the agency launched a project to assess the feasibility of collecting disaggregated performance data for its Maternal, Infant, and Early Childhood Home Visiting Program across relevant demographic and community variables, including by rural and underserved areas. HRSA noted that in September 2021, the agency awarded a contract to support this program's efforts to adjust its performance measures. In another example, HRSA directed its contractor who collects data on maternal health programs to create quantitative data collection tools and request that grantees report disaggregated data by race and ethnicity, when possible, and by geography type, such as urban and rural. With these disaggregated data, HRSA stated that the contractor will complete an annual data analysis. HRSA added that the agency will continue to engage with key stakeholders in the field on maternal health measurement to further support efforts to systematically disaggregate and analyze maternal health program data.
|
| Department of Health and Human Services | The Secretary of Health and Human Services should direct the Healthy People Maternal, Infant, and Child Health Workgroup and the Maternal Health Working Group to establish a formal coordinated approach for monitoring maternal health efforts across HHS, including in rural and underserved areas. Such an approach could include establishing a process for exchanging information and discussing relevant program efforts and outcomes across HHS during regular standing meetings on a routine basis. (Recommendation 3) |
HHS concurred with this recommendation and has taken steps to implement it. As of November 2021, HHS stated that the Healthy People Maternal, Infant, and Child Health Workgroup will report regularly to the Maternal Health Working Group by providing progress presentations on a quarterly basis beginning in January 2022. HHS noted that members of the two working groups plan to exchange information and discuss relevant program efforts and outcomes, including in rural and underserved areas, during meetings. For example, the Healthy People Maternal, Infant, and Child Health Workgroup will share data for Healthy People 2030 Maternal, Infant, and Child Health objectives broken out by available demographic groups, which are determined by the objectives' data sources.
|
