Substance Use Disorder: Medicaid Coverage of Peer Support Services for Adults
Fast Facts
Substance use disorders affected 19.3 million adults in the U.S. in 2018.
One treatment option for such disorders is services delivered by peer providers—individuals who use their own personal experiences recovering from substance use disorder to support others in their recovery.
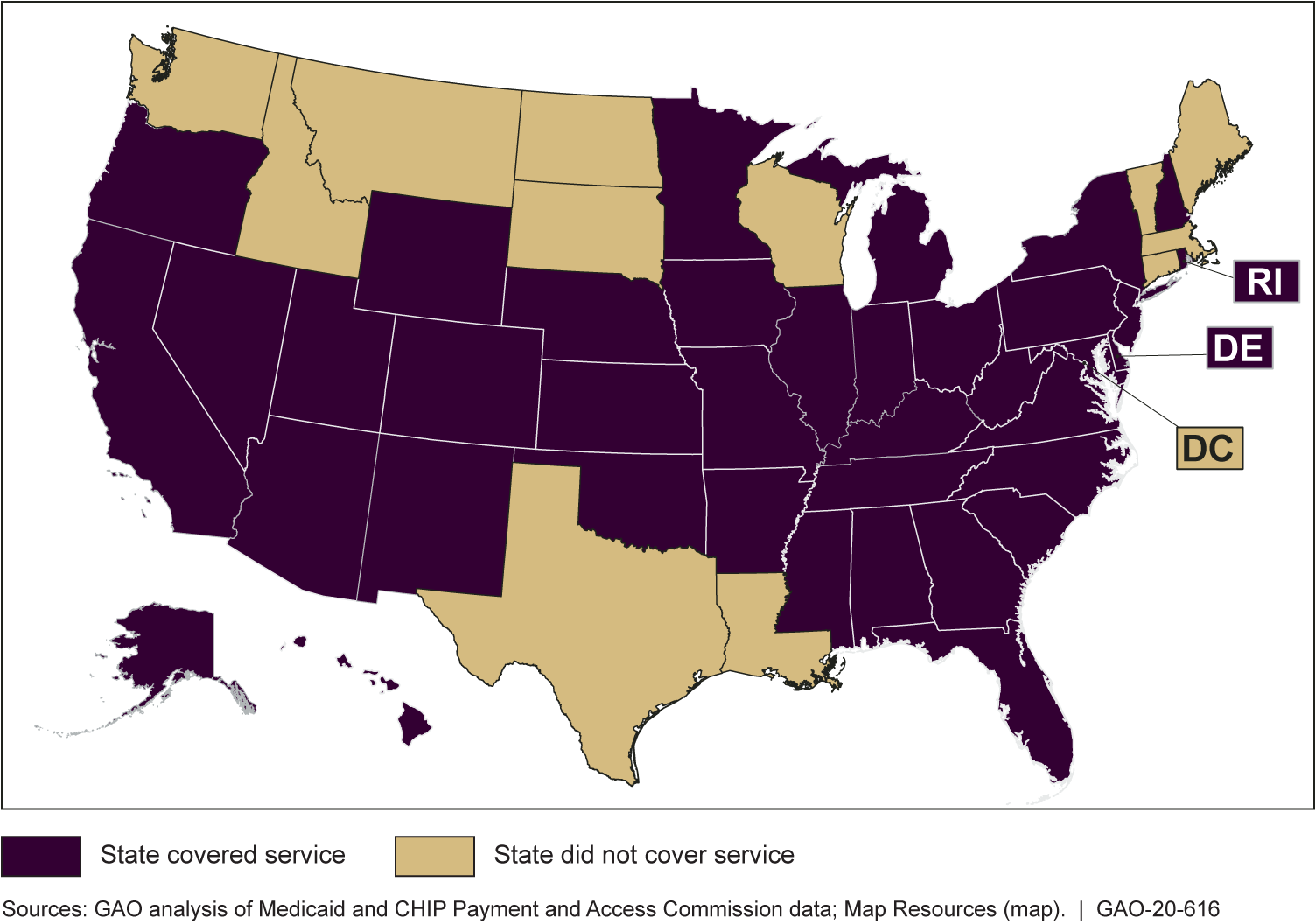
State Medicaid programs can choose to cover services offered by peer providers, but it is an optional benefit. We found that 37 states covered this benefit for adults with substance use disorder in 2018.
Medicaid Coverage of Peer Support Services for Adults with Substance Use Disorder, 2018

Highlights
What GAO Found
Substance use disorders (SUD)—the recurrent use of alcohol or illicit drugs causing significant impairment—affected about 19.3 million adults in the United States in 2018, according to the Substance Abuse and Mental Health Services Administration. State Medicaid programs have the option to cover services offered by peer providers—individuals who use their own lived experience recovering from SUD to support others in recovery. GAO's review of Medicaid and CHIP Payment and Access Commission data found that, in 2018, 37 states covered peer support services for adults with SUDs in their Medicaid programs.
Medicaid Coverage of Peer Support Services for Adults with Substance Use Disorders, 2018
Officials from the three states GAO reviewed—Colorado, Missouri, and Oregon—reported that their Medicaid programs offered peer support services as a complement, rather than as an alternative, to clinical treatment for SUD.
- Missouri officials said that peer providers did not maintain separate caseloads and were part of treatment teams, working in conjunction with doctors and other clinical staff. Similarly, officials in Colorado and Oregon said peer support services were only offered as part of a treatment plan.
- State officials reported that peer support services could be offered as an alternative to clinical treatment outside of Medicaid using state or grant funding.
Why GAO Did This Study
SUD treatment can help individuals reduce or stop substance use and improve their quality of life. In 2007, the Centers for Medicare & Medicaid Services recognized that peer providers could be an important component of effective SUD treatment, and provided guidance to states on how to cover peer support services in their Medicaid programs. However, states have flexibility in how they design and implement their Medicaid programs, and coverage for peer support services is an optional benefit.
The Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act included a provision for GAO to report on peer support services under Medicaid. This report describes, among other objectives, the extent to which state Medicaid programs covered peer support services for adult beneficiaries with SUDs nationwide, and how selected state Medicaid programs offered peer support services for adult beneficiaries with SUDs. GAO obtained state-by-state data from the Medicaid and CHIP Payment and Access Commission on 2018 Medicaid coverage of peer support services. GAO also reviewed information and interviewed officials from a nongeneralizable sample of three states, which GAO selected for a number of reasons, including to obtain variation in delivery systems used. The Department of Health and Human Services provided technical comments on a draft of this report, which GAO incorporated as appropriate.
For more information, contact Carolyn L. Yocom at (202) 512-7114 or yocomc@gao.gov.
