Science & Tech Spotlight: Social Distancing During Pandemics
Fast Facts
How far is far enough for successful social distancing? We take a look at some of the still-developing science behind the practice.
A CDC guideline based on historical studies of selected infections says that the area of highest risk is within 3 feet of an infected person. Some studies suggest a buffer of 6 feet may further reduce risk.
Other studies examining droplet dispersion in sneezing and coughing found they can go more than 6 feet. Also, viral material may persist in the air within a room for up to 3 hours.
But many factors, including the amount of viral material and duration of exposure needed to transmit the disease, are still unknown.
The distance droplets carry infectious materials depends on droplet size, humidity, air currents, and other factors.
Graphic showing distance different sized droplets can travel
Highlights
Why This Matters
Infectious diseases like COVID-19 can spread rapidly from person to person. Social distancing saves lives by slowing disease transmission and reducing the load on the health care system. The scientific research regarding effective social distancing practices continues to evolve.
The Science
What is it? Social distancing, also known as physical distancing, is the practice of maintaining physical distance from others and avoiding large gatherings, with the intent of reducing the rate of transmission of infectious diseases. COVID-19 has brought social distancing practices to the forefront worldwide as a means of controlling local spread of the disease.
How does it work? Practicing social distancing reduces the rate of new infections by limiting person-to-person transmission. This in turn can “flatten the curve,” by reducing the peak number of patients to levels the health care system can better manage, ultimately saving lives (fig. 1).
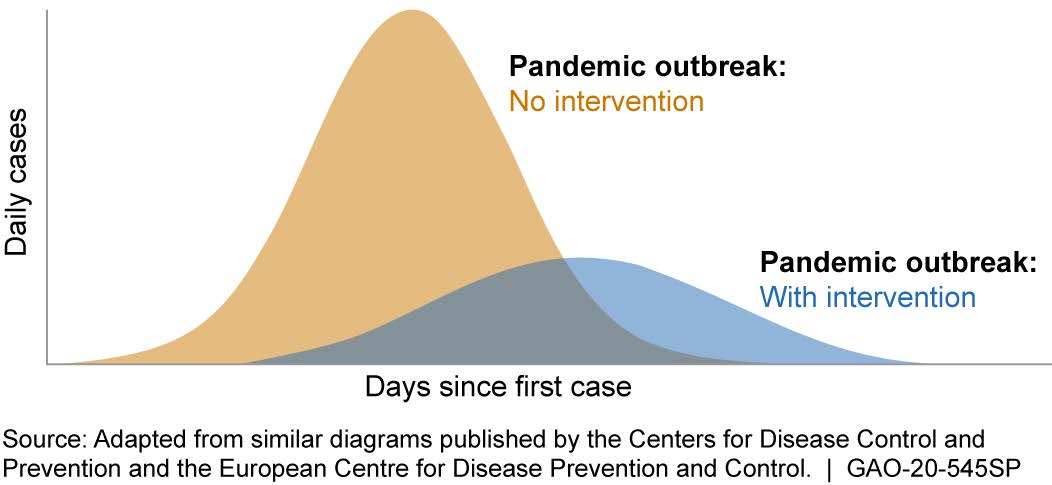
Figure 1. Reducing the rate of disease transmission through interventions, including social distancing and other measures, can alleviate the burden on medical facilities.
The success of social distancing depends on factors such as the distance that infectious particles can spread from a contagious person. The Centers for Disease Control and Prevention (CDC) currently recommends a 2 meter (about 6 feet) separation between people, while the World Health Organization (WHO) recommends 1 meter (about 3 feet).
The scientific basis for these recommendations comes from studies in fields such as fluid mechanics, epidemiology, and microbiology. For example, several studies estimated the velocity and distance traveled by droplets of different sizes expelled by sneezing, coughing, and breathing. These studies showed that sneezing and coughing can propel droplets more than 2 meters, with sneezing possibly propelling them further, and breathing less than 1 meter (fig. 2).
However, these estimates of speeds and distances are not absolute maximums. Coughing and sneezing are complex phenomena that are challenging to characterize precisely. And the behavior of droplets after they are expelled depends on their size, along with environmental factors such as humidity and air currents, making it challenging to be definitive about how far they may travel. Partly as a result of this ambiguity, social distancing guidelines are often conservative, recommending minimal personal contact except when necessary, such as within one’s own household.
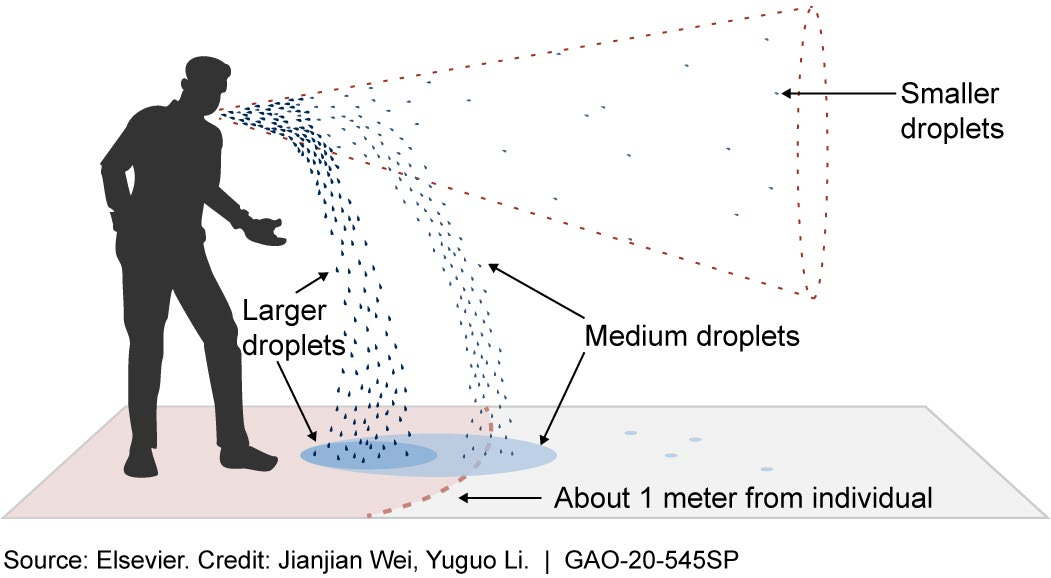
Figure 2. Droplets carrying infectious material can travel different distances, depending on factors such as size, humidity, and air currents.
Microbiological studies on a variety of respiratory viruses have shown viral material can travel 2 meters or farther from an infected patient. Specifically for COVID-19, one study showed that viral material can be recovered from ventilation fans in a patient’s room. However, it was not established whether the viral material could lead to disease transmission.
How mature is it? Some modeling studies of historical outbreaks suggest that social distancing is effective in reducing the spread of infections. For example, studies examining the use of social distancing during the 1918 influenza outbreak and the 2003 SARS outbreak showed such a reduction in part due to social distancing.
While it is clear that maintaining separation between individuals provides important protection, there is no definitive statement in the literature regarding effectiveness of specific distances. While a CDC guideline suggests that, historically, risk is highest within 1 meter of an infected person, the studies described above suggest a buffer of over 2 meters may further reduce risk. Still, several unknowns limit the ability to set specific guidance. For example, the risk from those droplets that travel long distances is unknown, as is the risk from viral material in aerosol form, which may persist for at least 3 hours in the air. Additionally, the amount of infectious material needed for COVID-19 transmission is not clear, nor is the effect of duration of exposure on risk, making it unclear how long two people standing 2 meters apart may safely interact. Social distancing practices, such as avoiding crowds and staying home, remain important, particularly as some infected people can shed virus before showing symptoms, according to WHO.
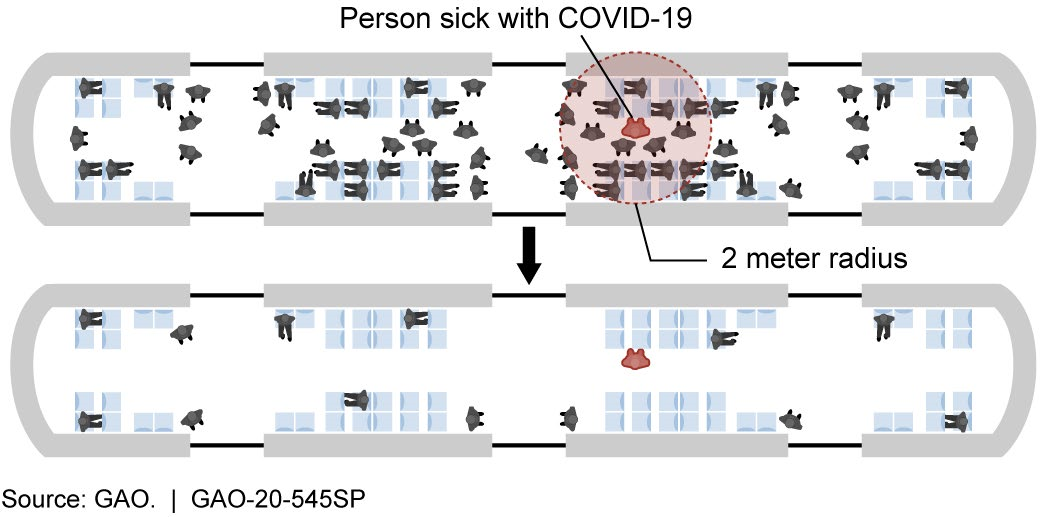 Figure 3. Determining the necessary spacing for effective social distancing, such as for riders in a subway car, can affect the extent of disease transmission. The shaded circle (top) shows the number of people who could be directly infected by droplets from a sick person.
Figure 3. Determining the necessary spacing for effective social distancing, such as for riders in a subway car, can affect the extent of disease transmission. The shaded circle (top) shows the number of people who could be directly infected by droplets from a sick person.
Opportunities
Social distancing offers opportunities to mitigate infectious disease spread. For example:
- Social distancing is readily deployable because it mainly requires authorities to disseminate directives and instructions. It does not require special equipment or medication to be distributed.
- It does not require special qualifications or extensive training for the public to do.
- It can be particularly important when no treatment or vaccine is available.
- It can be used to buy time for manufacturing and distributing protective supplies.
Challenges
- People may be reluctant or unable to practice social distancing, as it may be impossible for them to do, or adversely affect their daily routine and livelihood. Certain settings, such as onboard cruise ships or military vessels, can preclude some social distancing practices.
- There may be psychological impacts due to interruption of services such as mental health care to vulnerable populations, among other impacts.
- If implemented for long periods, social distancing may lead to large-scale disruptions in the economy, social cohesiveness, and the distribution of goods and services, which need to be considered in the context of public health assessments.
- Scientific studies to determine which distancing strategies are effective can be challenging, expensive, and risky, in part because some studies may test conditions that result in the spread of infection.
Policy Context and Questions
Social distancing, as a tool for public health response, raises a number of policy issues.
- How, when, and for how long can social distancing be broadly implemented and enforced effectively, while minimizing disruption to the daily routine of the populace and the economy?
- How can key complementary practices such as diagnostic testing best be used to inform the timing, location, and duration of social distancing?
- What research is needed to better establish the scientific basis of disease transmission so that effective methods for social distancing can be devised and promulgated, and who should conduct such research?
For more information, contact Karen Howard at 202-512-6888 or HowardK@gao.gov.
