Medicare Physician Services: Spending On and Use of Billing Codes for Comprehensive Care Planning Services
Fast Facts
A majority of Medicare's 39 million beneficiaries in 2017 had a serious condition, such as diabetes or heart disease. Treatment in these kinds of cases may require planning and coordination among an array of medical specialists.
We looked at how doctors and other health care providers bill Medicare for care planning and how much was spent on these services.
We found at least 58 Medicare codes providers can use to bill for some aspect of care planning—with 13 of them specifically for care planning. In 2017, spending on these 13 codes was about $467 million.

Doctor and patient
Highlights
What GAO Found
The 2018 Bipartisan Budget Act (BBA) defined longitudinal comprehensive care planning (LCCP) as services involving an interdisciplinary team of providers who develop and communicate a care plan to Medicare beneficiaries diagnosed with a serious or life-threatening illness. GAO identified at least 58 billing codes in Medicare's physician fee schedule that could be used by providers to bill for services that cover some or all of the LCCP service components as defined in the 2018 BBA —referred to by GAO as LCCP-type services. The 58 billing codes may be used individually or in combination, depending on a beneficiary's medical needs. Stakeholders representing providers told GAO their members generally use one or a combination of these codes to bill for LCCP-type services.
- Forty-five of the 58 codes are broadly-defined longstanding codes that can be used for LCCP-type services as well as other services such as the treatment of a specific medical complaint.
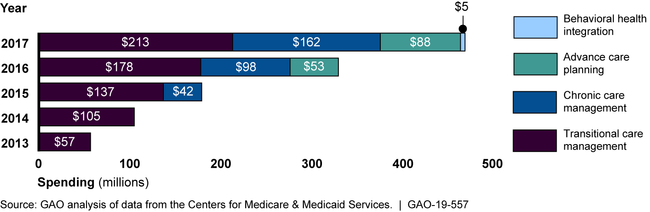
- The remaining 13 codes are more recent narrowly-defined codes introduced starting in 2013 that only cover LCCP-type services. They include transitional care management services introduced in 2013, chronic care management starting in 2015, advance care planning in 2016, and behavioral health integration in 2017.
GAO found that overall Medicare spending on LCCP-type services that were billed to the 58 codes increased from $26 billion in 2013 to almost $29 billion in 2017. While narrowly-defined services accounted for a small share of this total spending ($467 million in 2017), spending on these narrowly-defined services such as chronic care management increased rapidly. Moreover, spending growth on narrowly-defined services was driven by increased use of these services rather than increases in reimbursement rates. From 2013 through 2017, more beneficiaries received and more providers billed for narrowly-defined services. The number of Medicare beneficiaries receiving these services grew from about 267,000 to about 2.5 million. The number of providers billing these services grew from about 31,000 to about 100,000.
Medicare Spending on Narrowly-Defined Services, by Type of Service, 2013-2017
Why GAO Did This Study
Medicare's physician fee schedule contains over 8,000 billing codes for office visits, surgical procedures, or other services provided to beneficiaries. Some provider groups have concerns that these codes do not sufficiently account for the LCCP-type services they provide to Medicare beneficiaries with complex medical needs.
The BBA included a provision that GAO examine billing codes that may be used for LCCP-type services for beneficiaries with a serious or life-threatening illness.
GAO identified, among other things, (1) existing Medicare physician fee schedule billing codes that can be used to bill LCCP-type services; and (2) trends in Medicare spending on these services from 2013 through 2017.
GAO reviewed Centers for Medicare & Medicaid Services (CMS) billing code manuals and American Medical Association (AMA) code descriptors to identify existing codes containing key components of LCCP-type services; analyzed Medicare Part B claims data from 2013 to 2017 (the most recent available at the time of GAO's review); and interviewed officials from CMS and 19 stakeholders, including the AMA, national physician groups, and other provider groups that had previously given input on the topic to Congress.
GAO provided a draft of this report to the Department of Health and Human Services (HHS). In response, HHS provided technical comments, which GAO incorporated as appropriate.
For more information, contact Jessica Farb at (202) 512-7114 or farbj@gao.gov.
