Health Information Technology: Approaches and Challenges to Electronically Matching Patients' Records across Providers
Fast Facts
Health care providers increasingly share records electronically. It can be hard to match records to the right patient, and mistakes can have consequences. For example, a doctor might use information from the wrong record when treating a patient.
Inaccurate, incomplete, or inconsistently formatted data can make record-matching difficult. These data problems can happen for many reasons, e.g., a patient can go by a full name in one record and a nickname in another.
We explored possible solutions, such as requiring a specific format for recording a patient’s name and address, and sharing best practices for record-matching.
Examples of how demographic information in medical records can vary among providers
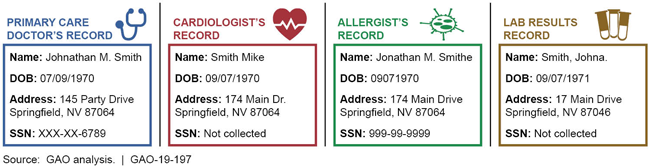
Examples include SSN in primary care and allergist's records but not in cardiologist's or with lab results
Highlights
What GAO Found
Stakeholders GAO interviewed, including representatives from physician practices and hospitals, described their approaches for matching patients' records—that is, comparing patient information in different health records to determine if the records refer to the same patient. Stakeholders explained that when exchanging health information with other providers, they match patients' medical records using demographic information, such as the patient's name, date of birth, or sex. This record matching can be done manually or automatically. For example, several provider representatives said that they rely on software that automatically matches records based on the records' demographic information when receiving medical records electronically. Stakeholders said that software can also identify potential matches, which staff then manually review to determine whether the records correspond to the same patient. Stakeholders also said that inaccurate, incomplete, or inconsistently formatted demographic information in patients' records can pose challenges to accurate matching. They noted, for example, that records don't always contain correct information (e.g., a patient may provide a nickname rather than a legal name) and that health information technology (IT) systems and providers use different formats for key information such as names that contain hyphens.
Stakeholders GAO interviewed identified recent or ongoing efforts to improve the data and methods used in patient record matching, such as the following:
Several stakeholders told GAO they worked to improve the consistency with which they format demographic data in their electronic health records (EHR). In 2017, 23 providers in Texas implemented standards for how staff record patients' names, addresses, and other data. Representatives from three hospitals said this increased their ability to match patients' medical records automatically. For example, one hospital's representatives said they had seen a significant decrease in the need to manually review records that do not match automatically.
Stakeholders also described efforts to assess and improve the effectiveness of methods used to match patient records. For example, in 2017 the Office of the National Coordinator for Health Information Technology (ONC) hosted a competition for participants to create an algorithm that most accurately matched patient records. ONC selected six winning submissions and plans to report on their analysis of the competition's data.
Stakeholders said more could be done to improve patient record matching, and identified several efforts that could improve matching. For example, some said that implementing common standards for recording demographic data; sharing best practices and other resources; and developing a public-private collaboration effort could each improve matching. Stakeholders' views varied on the roles ONC and others should play in these efforts and the extent to which the efforts would improve matching. For example, some said that ONC could require demographic data standards as part of its responsibility for certifying EHR systems, while other stakeholders said that ONC could facilitate the voluntary adoption of such standards. Multiple stakeholders emphasized that no single effort would solve the challenge of patient record matching.
Why GAO Did This Study
Health care providers are increasingly sharing patients' health records electronically. When a patient's records are shared with another provider, it is important to accurately match them to the correct patient. GAO and others have reported that accurately matching patient health records is a barrier to health information exchange and that inaccurately matched records can adversely affect patient safety or privacy. At the federal level, ONC is charged with coordinating nationwide efforts to implement and use health IT.
The 21st Century Cures Act included a provision for GAO to study patient record matching. In this report, GAO describes (1) stakeholders' patient record matching approaches and related challenges; and (2) efforts to improve patient record matching identified by stakeholders.
To do its work, GAO reviewed reports by ONC and others about patient record matching. GAO also interviewed various stakeholders that play a role in exchanging health records, including representatives from physician practices, hospitals, health systems, health information exchange organizations, and health IT vendors. GAO also interviewed other stakeholders, such as ONC officials, provider and industry associations, and researchers. GAO selected stakeholders based on background research and input from other stakeholders, and interviewed 37 stakeholders in total. The information from stakeholders is not generalizable. HHS provided technical comments on a draft of this report, which GAO incorporated as appropriate.
For more information, contact Jessica Farb at (202) 512-7114 or farbj@gao.gov.
