Medicare Advantage: Benefits and Challenges of Payment Adjustments Based on Beneficiaries' Ability to Perform Daily Tasks
Fast Facts
Medicare Advantage (MA) is a private-plan alternative to traditional Medicare. Medicare pays MA plans a monthly amount per beneficiary, and this amount is adjusted based on a beneficiary’s health status, among other things. As such, Medicare generally pays an MA plan more for a beneficiary in poorer health (who will likely have higher health care costs) than for a beneficiary in better health.
We found that these payment adjustments could be improved if they accounted for beneficiaries’ ability to perform daily tasks (e.g., bathing or dressing), though doing so could be quite challenging, in part because this information is not readily available.

Photo of an elderly person's hands.
Highlights
What GAO Found
The Centers for Medicare & Medicaid Services (CMS) pays Medicare Advantage (MA) plans a monthly capitated amount to provide coverage for enrolled beneficiaries. This amount is adjusted to reflect beneficiary health status, a process known as risk adjustment. Beneficiaries in poorer health are generally expected to use more health care services than beneficiaries in better health; thus, risk adjustment pays more to MA plans for beneficiaries in poorer health to compensate. CMS's risk adjustment model estimates health care spending based on beneficiary demographic characteristics and clinical diagnoses. However, this model does not account for functional status—the ability to perform routine daily activities such as bathing or dressing. GAO estimated that about 4 in 10 beneficiaries had functional limitations in 2016.
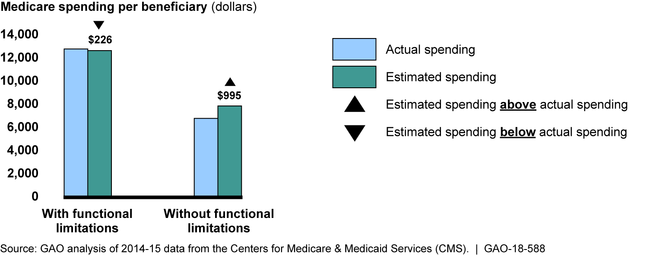
GAO found that for the sample of beneficiaries analyzed, the MA risk adjustment model underestimated spending for those with functional limitations and overestimated spending for those without such limitations. These findings suggest that risk adjustment accuracy could be improved by accounting for functional status, which could in turn reduce any financial disadvantages plans may experience by enrolling beneficiaries with functional limitations.
Average Actual and Estimated Medicare Spending for a Sample of Beneficiaries under CMS's Current Risk Adjustment Model, by Functional Status, 2015
GAO also found that CMS and other stakeholders could face substantial challenges if the risk adjustment model were revised to account for beneficiary functional status, in part because this information is not readily available. For example, about three-fourths of beneficiaries do not receive health care in settings where functional status information is routinely collected. Stakeholders told GAO that expanding the collection of such information could be resource intensive for CMS, plans and health care providers, and an imposition for some beneficiaries. In addition, the potential for higher payments may give MA plans a financial incentive to identify beneficiaries with functional limitations. If this incentive causes MA plans to identify functional limitations more completely than providers in fee-for-service (FFS) Medicare, the risk adjustment process would need to account for this to avoid inappropriately high payments to plans because the risk adjustment model is estimated based on FFS data.
Why GAO Did This Study
Accurate risk adjustment avoids the creation of a financial advantage or disadvantage for plans solely on the basis of the health status of enrolled beneficiaries. The 21st Century Cures Act contains a provision for GAO to report on issues related to incorporating functional status into MA risk adjustment.
Among other reporting objectives, this report examines (1) the accuracy of the current CMS risk adjustment model for beneficiaries with functional limitations and the potential benefits of accounting for functional status in MA risk adjustment; and (2) the potential challenges of accounting for functional status in risk adjustment. GAO analyzed 2014 data on diagnoses and survey data on functional status for a sample of community-residing FFS beneficiaries to estimate 2015 spending based on CMS's current risk adjustment model. GAO compared those estimates to actual 2015 total health care spending—the most recent year for which summarized data on beneficiary spending were available at the time of GAO's analysis. While the survey was designed to be representative of all FFS beneficiaries, the sample GAO analyzed may not be representative of FFS beneficiaries who reside in the community in part because it was restricted to those who provided complete functional status survey information. GAO also reviewed CMS guidance documents and interviewed stakeholders, industry experts, and CMS officials. The Department of Health and Human Services provided technical comments on a draft of this report, which GAO incorporated as appropriate.
For more information, contact James Cosgrove at (202) 512-7114 or cosgrovej@gao.gov.
