Medicare: Increasing Hospital-Physician Consolidation Highlights Need for Payment Reform
Highlights
What GAO Found
Vertical consolidation is a financial arrangement that occurs when a hospital acquires a physician practice and/or hires physicians to work as salaried employees. The number of vertically consolidated hospitals and physicians increased from 2007 through 2013. Specifically, the number of vertically consolidated hospitals increased from about 1,400 to 1,700, while the number of vertically consolidated physicians nearly doubled from about 96,000 to 182,000. This growth occurred across all regions and hospital sizes, but was more rapid in recent years. After hospitals and physicians vertically consolidate, services performed in physician offices, such as evaluation & management (E/M) office visits, can be classified as being performed in hospital outpatient departments (HOPD). Medicare often pays providers at a higher rate when the same service is performed in an HOPD rather than in a physician office. For example, in 2013, the total Medicare payment rate for a mid-level E/M office visit for an established patient was $51 higher when the service was performed in an HOPD instead of a physician office.
Number of Vertically Consolidated Hospitals and Physicians, 2007–2013
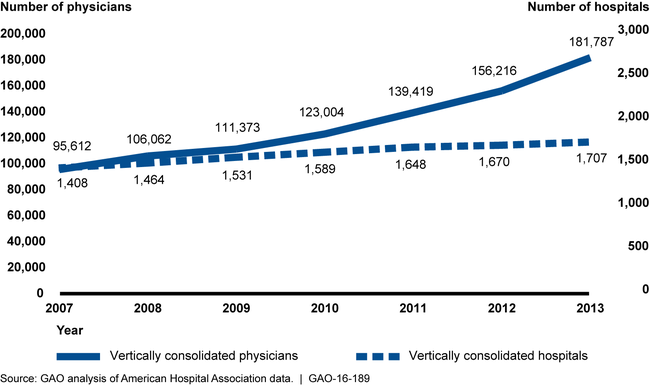
Note: This analysis was limited to hospitals that served Medicare beneficiaries.
The percentage of E/M office visits—as well as the number of E/M office visits per beneficiary—performed in HOPDs, rather than in physician offices, was generally higher in counties with higher levels of vertical consolidation in 2007 through 2013. For example, the median percentage of E/M office visits performed in HOPDs in counties with the lowest levels of vertical consolidation was 4.1 percent in 2013. In contrast, this rate was 14.1 percent for counties with the highest levels of consolidation. GAO's findings suggest that Medicare will likely pay more than necessary for E/M office visits. Such excess payments are inconsistent with Medicare's role as an efficient purchaser of health care services. However, the Centers for Medicare & Medicaid Services (CMS)—the agency that is responsible for the Medicare program—lacks the statutory authority to equalize total payment rates between HOPDs and physician offices and achieve Medicare savings.
Why GAO Did This Study
Medicare expenditures for HOPD services have grown rapidly in recent years. Some policymakers have raised questions about whether this growth may be attributed to services that were typically performed in physician offices shifting to HOPDs. GAO was asked to examine trends in vertical consolidation and its effects on Medicare.
This report examines, for years 2007 through 2013, (1) trends in vertical consolidation between hospitals and physicians and (2) the extent to which higher levels of vertical consolidation were associated with more E/M office visits being performed in HOPDs. GAO analyzed, using various methods including regression analyses, the most recent available claims data from CMS and survey data from the American Hospital Association, in which hospitals report the types of financial arrangements they have with physicians.
Recommendations
In order to prevent the shift of services from lower paid settings to the higher paid HOPD setting from increasing costs for the Medicare program and beneficiaries, Congress should consider directing the Secretary of the Department of Health and Human Services (HHS) to equalize payment rates between settings for E/M office visits—and other services that the Secretary deems appropriate—and to return the associated savings to the Medicare program. HHS provided technical comments on a draft of this report, which GAO incorporated as appropriate.
Matter for Congressional Consideration
| Matter | Status | Comments |
|---|---|---|
| In order to prevent the shift of services from physician offices to HOPDs from increasing costs for the Medicare program and beneficiaries, Congress should consider directing the Secretary of HHS to equalize payment rates between settings for E/M office visits--and other services that the Secretary deems appropriate--and to return the associated savings to the Medicare program. | A bill (H.R.5378) passed by the House of Representatives in December 2023 during the 118th Congress would have equalized payments for certain drug administration services at off-campus hospital outpatient departments, partially addressing GAO's December 2015 recommendation. As of February 2025, no additional legislative action has been identified in the 119th Congress that would address GAO's recommendation. The Bipartisan Budget Act of 2015, enacted in November 2015, partially addressed our recommendation as it limits certain providers from billing at higher hospital outpatient department payment rates. Specifically, the legislation excludes services furnished by off-campus hospital outpatient departments from reimbursement under Medicare's hospital outpatient prospective payment system, effective January 1, 2017. According to the Congressional Budget Office, this action saves the Medicare program $9.3 billion over 10 years. However, the Act does not apply to services furnished by providers billing as hospital outpatient departments prior to enactment of the legislation-which includes providers billing as hospital outpatient departments during the study period in our report-as well as hospital outpatient departments located on hospital campuses. This means that, even in 2017 and beyond, many providers will not be affected by the Act, and Medicare will continue to pay more than necessary for certain services. In November 2018, CMS issued a final rule adopting payment changes-that have since been partially overturned under a decision by a federal district court, which CMS has appealed-capping payment rates for certain services furnished by the off-campus hospital outpatient departments that existed or were under construction in 2015 at the physician fee schedule rate. Since these services furnished by these off-campus hospital outpatient departments were paid at a higher rate, the payment cap, which was to be implemented over 2 years, was intended to equalize payment rates for certain clinical visits between settings where services can be provided, for example, physician offices. In 2019, CMS applied 50 percent of the payment reduction and in 2020 and subsequent years planned to apply 100 percent of the payment reduction. The rule applied to specific clinical visits, where other services would continue to be paid at the higher rate. In response to a lawsuit challenging CMS's authority to issue the November 2018 rule, a federal court of appeals ruled in July 2020 that CMS had the authority to adopt these payment changes. An appeal of that ruling was filed, and in June 2021, the Supreme Court declined to take up the case. In order to fully implement this recommendation, Medicare payment rates for evaluation and management services should be equalized for all hospital outpatient departments, regardless of whether they are deemed on-campus or off-campus. |
