Rural Hospital Closures: Affected Residents Had Reduced Access to Health Care Services
Fast Facts
Rural hospitals provide essential health care to rural communities. Yet, over 100 rural hospitals closed from January 2013-February 2020.
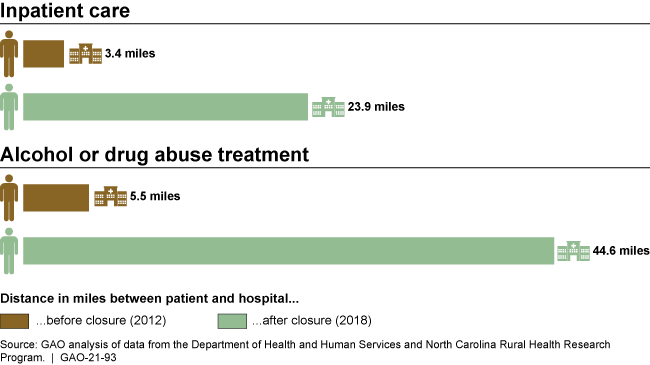
When rural hospitals closed, people living in areas that received health care from them had to travel farther to get the same health care services—about 20 miles farther for common services like inpatient care. People had to travel even farther—about 40 miles—for less common services like alcohol or drug abuse treatment.
Before rural hospitals closed, counties where these hospitals were located had fewer doctors than counties without any closures. The number of doctors further decreased when hospitals closed.
People had to travel farther to get health care services after rural hospitals closed in their areas.
Highlights
What GAO Found
GAO found that when rural hospitals closed, residents living in the closed hospitals' service areas would have to travel substantially farther to access certain health care services. Specifically, for residents living in these service areas, GAO's analysis shows that the median distance to access some of the more common health care services increased about 20 miles from 2012 to 2018. For example, the median distance to access general inpatient services was 3.4 miles in 2012, compared to 23.9 miles in 2018—an increase of 20.5 miles. For some of the less common services that were offered by a few of the hospitals that closed, this median distance increased much more. For example, among residents in the service areas of the 11 closed hospitals that offered treatment services for alcohol or drug abuse, the median distance was 5.5 miles in 2012, compared to 44.6 miles in 2018—an increase of 39.1 miles to access these services (see figure).
Median Distance in Miles from Service Areas with Rural Hospital Closures to the Nearest Open Hospital that Offered Certain Health Care Services, 2012 and 2018
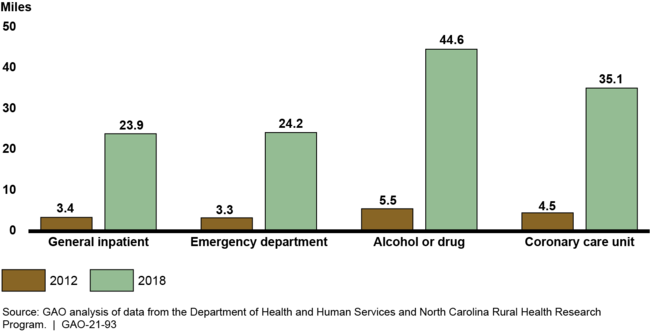
Notes: GAO focused its analysis on the health care services offered in 2012 by the 64 rural hospitals that closed during the years 2013 through 2017 and for which data were available. For example, in 2012, 64 closed hospitals offered general inpatient services, 62 offered emergency department services, 11 offered treatment services for alcohol or drug abuse, and 11 offered services in a coronary care unit. To examine distance, GAO calculated “crow-fly miles” (the distance measured in a straight line) from the geographic center of each closed rural hospital's service area to the geographic center of the ZIP Code with the nearest open rural or urban hospital that offered a given service.
GAO also found that the availability of health care providers in counties with rural hospital closures generally was lower and declined more over time, compared to those without closures. Specifically, counties with closures generally had fewer health care professionals per 100,000 residents in 2012 than did counties without closures. The disparities in the availability of health care professionals in these counties grew from 2012 to 2017. For example, over this time period, the availability of physicians declined more among counties with closures—dropping from a median of 71.2 to 59.7 per 100,000 residents—compared to counties without closures—which dropped from 87.5 to 86.3 per 100,000 residents.
Why GAO Did This Study
Rural hospitals face many challenges in providing essential access to health care services to rural communities. From January 2013 through February 2020, 101 rural hospitals closed.
GAO was asked to examine the effects of rural hospital closures on residents living in the areas of the hospitals that closed. This report examines, among other objectives, how closures affected the distance for residents to access health care services, as well as changes in the availability of health care providers in counties with and without closures.
GAO analyzed data from the Department of Health and Human Services (HHS) and the North Carolina Rural Health Research Program (NC RHRP) for rural hospitals (1) that closed and those that were open during the years 2013 through 2017, and (2) for which complete data generally were available at the time of GAO's review. GAO also interviewed HHS and NC RHRP officials and reviewed relevant literature.
GAO defined hospitals as rural according to data from the Federal Office of Rural Health Policy. GAO defined hospital closure as a cessation of inpatient services, the same definition used by NC RHRP. GAO defined service areas with closures as the collection of ZIP Codes that were served by closed rural hospitals and service areas without closures as the collection of ZIP Codes served only by rural hospitals that were open.
GAO provided a draft of this report to HHS for comment. The Department provided technical comments, which GAO incorporated as appropriate.
For more information, contact James Cosgrove at (202) 512-7114 or cosgrovej@gao.gov.
