Science & Tech Spotlight: Coronaviruses
Fast Facts
A December 2019 outbreak of a new coronavirus, COVID-19, has seen a high infection rate and a mortality rate of about 3%, as of February 2020.
Coronaviruses are most commonly transmitted by coughing, sneezing, person-to-person contact, and touching objects that have viral particles on them, according to CDC. The best prevention is washing hands with soap and avoiding close contact with the sick and with quarantine workers.
This spotlight gives an overview of coronaviruses and looks at:
Previous coronavirus outbreaks
How coronaviruses work
Current diagnostics
Research on vaccines and therapeutics
coronavirus
Highlights
Why This Matters
Coronaviruses can spread rapidly and cause outbreaks with high mortality rates. They were not considered a major risk for humans until the SARS outbreak in 2002. Since then, there have been multiple highly contagious outbreaks originating in animals and spreading to humans—most recently the outbreak in Wuhan, China of Coronavirus Disease 2019 (COVID-19).
The Technology
What is it? While the outbreak of COVID-19 in China has brought the term coronavirus into daily usage, coronaviruses can vary in severity. They can cause respiratory issues, such as pneumonia, and are believed to be one cause of the common cold. According to the Centers for Disease Control and Prevention (CDC), most people will be infected by a coronavirus at some point in their lifetimes. As of March 2020, seven coronaviruses have been identified that can cause illness in humans. Most infections result in mild to moderate symptoms, such as runny nose, headache, cough, sore throat, fever, and a run-down feeling.
Coronaviruses are most commonly transmitted by coughing, sneezing, person-to-person contact, and touching objects that have viral particles on them, according to CDC. The best prevention is washing hands with soap and avoiding contact with people who are sick or work in quarantine areas. Current treatment methods are limited, and research is being fast-tracked to develop a vaccine against existing and emerging coronaviruses.
Recent high-profile coronavirus outbreaks have raised new concern because of high mortality rates relative to the coronaviruses that cause the common cold. In addition, the severe coronaviruses can cause both upper- and lower-respiratory-tract infections, including pneumonia.
Since 2002, there have been three severe outbreaks of respiratory illness caused by coronaviruses, all three originating in animals. In 2002, an outbreak of Severe Acute Respiratory Syndrome (SARS) began in China and had a mortality rate of approximately 10 percent. In 2012, an outbreak of Middle East Respiratory Syndrome (MERS) had a mortality rate reported as high as 34 percent. Most recently, a December 2019 outbreak of a new coronavirus, SARS-CoV-2—which causes COVID-19—has seen a high infection rate, with over 70,000 infected and over 2,600 deaths—a mortality rate of approximately 3 percent as of February 24th, 2020, according to the World Health Organization (WHO). Estimates of the reproductive ratio, or R0, for COVID-19 have also indicated that it has the potential to spread rapidly. These estimates are tentative, however, because the R0 is a complex epidemiologic measure that is context-specific and affected by numerous biological, behavioral, and environmental factors.
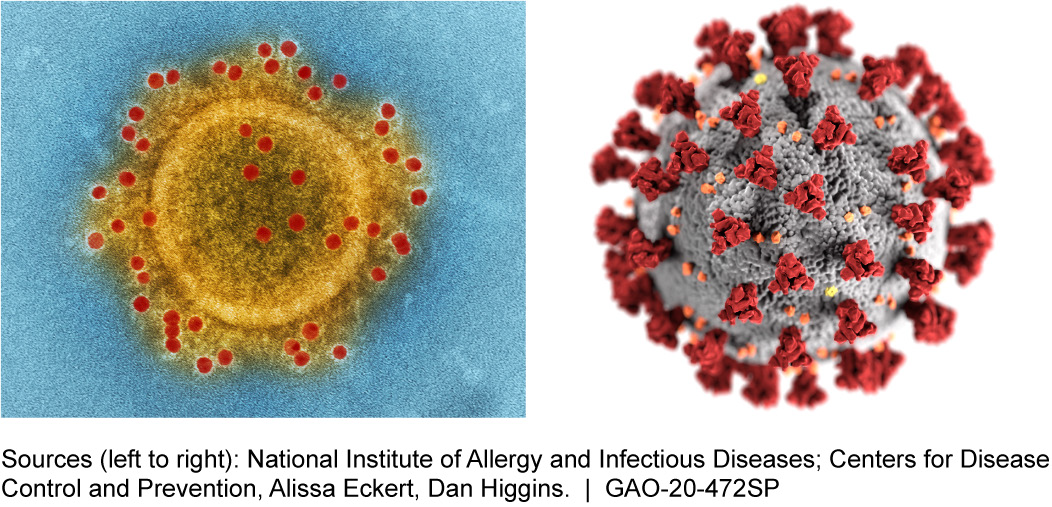
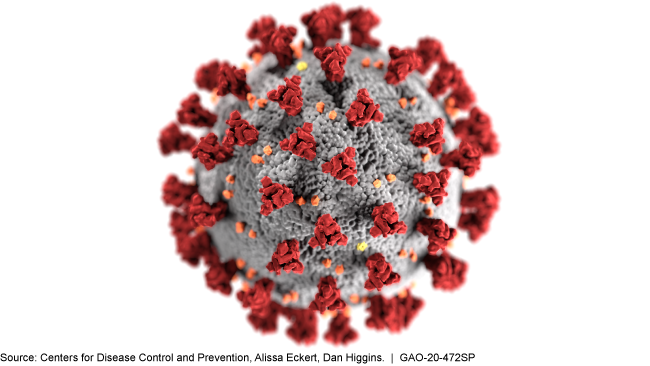
Figure 1.Electron microscope image and schematic of coronavirus particles (Middle East Respiratory Syndrome Coronavirus and general coronavirus respectively).
How does it work? Coronaviruses are believed to work in similar ways. Viral particles attach themselves to specific molecules, known as receptors, on the surface of a human or animal cell, allowing the virus to enter. Once inside, the virus discards its outer coating, releasing its genetic material into the host cell. This can occur in many cells at the same time. The virus can then use the cell’s own mechanisms—for example, the mechanism to produce proteins based on genetic code—to replicate itself. The hijacking of the cell’s functions causes the release of new viral particles and restarting the process, either in more cells of the same host or in another host that becomes infected.
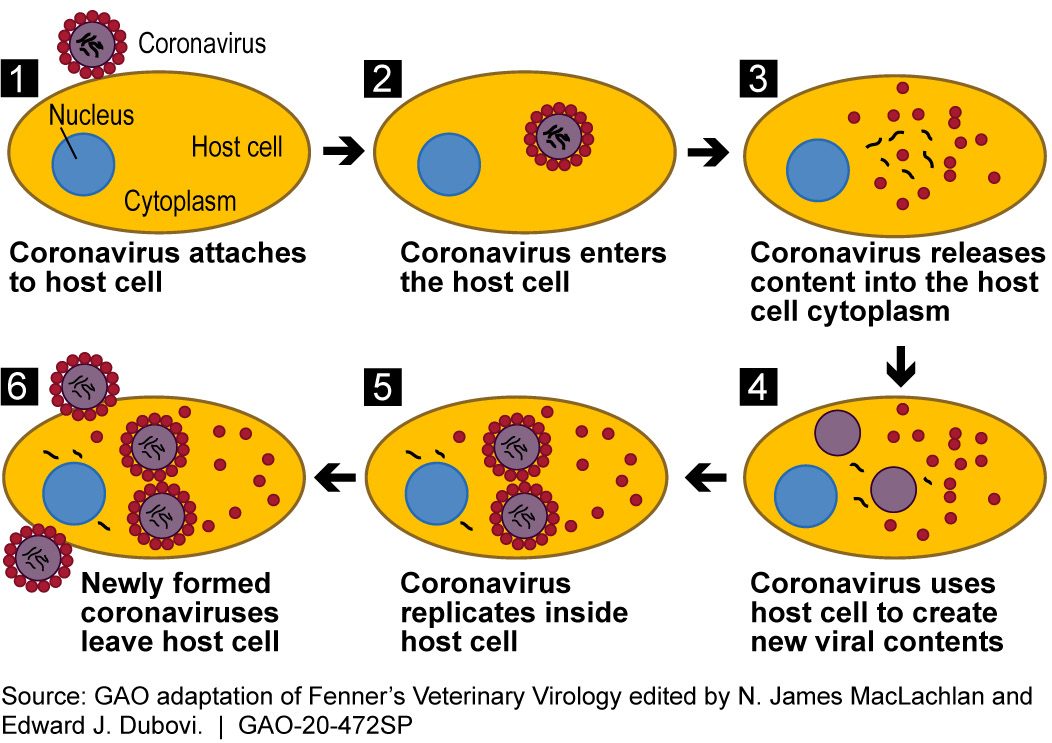
Figure 2. Schematic of how a coronavirus infects host cells. This process is similar for all RNA viruses, the large class to which coronaviruses belong.
Coronaviruses mutate rapidly compared to other viruses, enabling them to adapt to new environments. Coronaviruses are ribonucleic acid (RNA) viruses, which are more prone to random mutations than deoxyribonucleic acid (DNA) viruses. Because DNA viruses, like chickenpox and many others, are more stable, it is easier to create long term effective vaccines against them. In contrast, RNA viruses, like flu, may regularly require new vaccines.
Generally, coronaviruses originate in animals, with the most likely origin being bats, and can spread from animal to animal. In environments where humans and multiple animal species mix, such as live animal markets and farms, there is an increased likelihood that a coronavirus can mutate and spread into humans. The original animal vector for SARS-CoV-2 has not yet been determined.
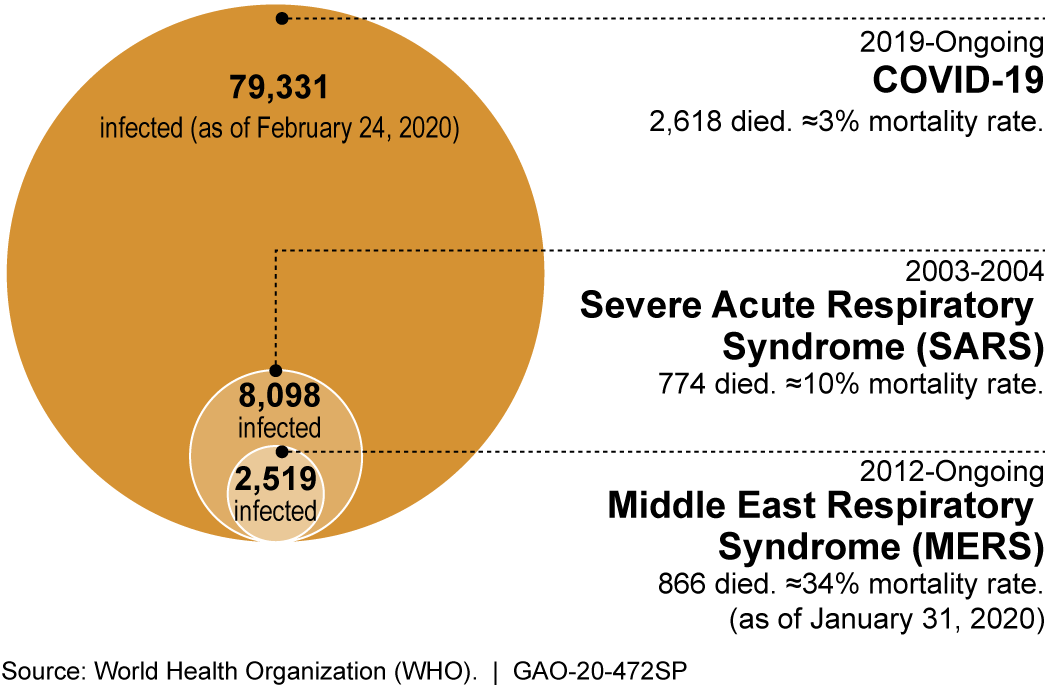
Figure 3. The recent outbreaks of coronavirus-caused diseases known to infect humans (COVID-19 numbers are confirmed and as reported by China).
How mature are diagnostics and therapies?
Several procedures, including diagnostic testing, are available to address coronaviruses, and are being used in the U.S. response. However, vaccines and therapies are not yet mature.
In the wake of the COVID-19 outbreak, Chinese researchers isolated the virus, sequenced its genome, and shared the results with the scientific community. The sequencing allowed CDC to develop a diagnostic test that is now being distributed to local labs. Also, based on genetic similarities, a vaccine developed for SARS has been recommended by researchers as a possible option for SARS-CoV-2. And researchers are drawing on the SARS-CoV-2 genome to help determine which aspects of the coronavirus might be used to develop a more specific vaccine against it.
For those already infected, doctors are trying a drug originally made to treat Ebola that also works against SARS and MERS. The first U.S. patient diagnosed with COVID-19 was treated with this drug under compassionate use (a policy allowing some use of non-approved drugs), and additional antivirals are being tested.
Opportunities
- Identification of common targets in coronaviruses to develop vaccines against all coronaviruses.
- Increased coordination by industry, academia, and government could improve awareness of treatment options for future outbreaks.
- Advances in predictive infectious disease modelling to better inform decisions about interventions in future outbreaks.
Challenges
- For rapid deployment, potential treatments need to be prepared prior to an outbreak despite limited information and incentives.
- Development of vaccines for RNA viruses requires frequent evaluation and reformulation. It is complex, costly, and time consuming.
- Outbreak detection requires constant monitoring and coordination among nations, which can be impeded by more closed societies.
- Global economic consequences of such outbreaks can be serious. According to multiple economic forecasting models, SARS cost the global economy $30-100 billion.
Policy Context and Questions
- To what extent are surveillance and clinical data, computational models, and information sharing mechanisms in place to promote agile and effective risk management during disease outbreaks?
- What policies and mechanisms are in place or needed to help maintain medical supply chains during global disease outbreaks?
For more information, contact Tim Persons at 202-512-6888 or personst@gao.gov.
