VA Health Care: Improved Communication about Available Data Needed to Enhance the HIV Screening Process
Fast Facts
The Veterans Health Administration is the largest single provider of medical care to HIV infected individuals in the nation. VA medical centers in 2018 provided care to over 31,000 HIV-positive veterans. Those who receive health care before their infections progress have better health, longer lives, and a lower chance of transmitting HIV.
Among other things, we found VA does not track whether HIV-positive veterans began treatment within 30 days of their diagnosis—VA’s recommended maximum. We recommended that VA communicate to key VA staff whether veterans are being linked to care in the recommended period.

Veteran Affairs Medical Center building
Highlights
What GAO Found
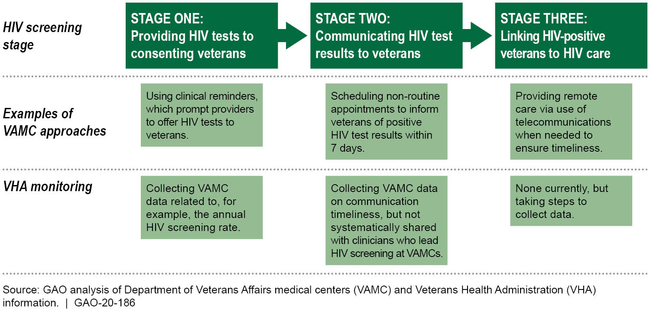
Officials from five selected Department of Veterans Affairs (VA) medical centers (VAMC) reported using various approaches to facilitate human immunodeficiency virus (HIV) screening, which involves three stages. For example, for the first stage of HIV screening (providing HIV tests to consenting veterans), officials told GAO that VAMCs use information technology solutions, such as clinical reminders that prompt providers to offer HIV tests to veterans who have not been tested. These clinical reminders can also prompt providers to offer an HIV test on a repeated, rather than a one-time, basis to veterans with known higher risk factors for acquiring HIV.
|
Examples of VAMC Approaches and VHA Monitoring for Human Immunodeficiency Virus (HIV) Screening
|
The Veterans Health Administration (VHA) monitors the first stage of HIV screening by collecting and disseminating data that VAMCs can use to calculate and, if necessary, improve facility HIV testing rates. VHA also collects data on the time frames in which results for eight types of tests are communicated to veterans; these data could indicate how timely test results are being communicated generally (stage two of HIV screening). However, VHA has not effectively communicated the availability of these data to HIV lead clinicians. In addition, VHA does not currently monitor whether VAMCs link veterans who test positive for HIV to care in a timely manner (stage three of HIV screening). VHA officials indicated that they are in the process of building the capacity to collect and disseminate to HIV lead clinicians data on the number of veterans at each VAMC who are linked to HIV care within 30 days, as recommended. However, the time frames for completing these efforts have been extended due to competing priorities, such as implementing required improvements in the diagnosis and treatment of veterans with Hepatitis C. Until VHA improves VAMC staff's access to, or provides them with, these data, it increases its risk that HIV-positive veterans do not receive timely treatment. Such treatment can improve veterans' health outcomes and prevent the transmission of the virus to others.
Why GAO Did This Study
VHA is the largest single provider of medical care to HIV infected individuals in the nation. In 2018, VAMCs tested approximately 240,000 veterans for HIV and provided HIV care to over 31,000 veterans. Early diagnosis and timely treatment is important for achieving favorable health outcomes and reducing the risk of transmitting the virus to others.
The accompanying Joint Explanatory Statement for the Consolidated Appropriations Act, 2018 included a provision for GAO to examine how VAMCs have implemented VHA's HIV screening policy. This report examines (1) approaches that selected VAMCs use to facilitate HIV screening, and (2) the extent to which VHA monitors HIV screening. GAO analyzed VHA documents, including VHA directives and a nongeneralizable sample of 103 veterans' medical records, to understand how providers made decisions and documented actions related to HIV screening. GAO also interviewed VHA and VAMC officials, the latter from five facilities selected based on factors such as the range of HIV prevalence rates.
Recommendations
VA should (1) improve communication regarding the availability of data on the timeliness with which test results are communicated to veterans, and (2) disseminate data to HIV lead clinicians on the timeliness with which veterans are linked to HIV care. VA concurred with GAO's recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Department of Veterans Affairs | The Under Secretary for Health should take steps to improve communication to VAMC staff (including HIV lead clinicians) about the availability of data on the time frames in which test results are communicated to veterans. (Recommendation 1) |
VHA concurred with this recommendation and provided regular updates on its progress in implementing it. In March 2020, officials from the Office of Primary Care (OPC) and other VHA offices presented during the Patient Aligned Care Team Community of Practice's monthly call on the topic of communicating test results. They provided timelines in which test results are to be communicated to patients, along with instructions for accessing External Peer Review Program (EPRP) data on the communication of test results, including the time frames in which HIV test results are communicated to veterans. Later that month, OPC sent an email to the VHA Performance Measurement News Listserv announcing the availability of EPRP data, and in June 2020, OPC made another announcement in a Chief Medical Officer and Quality Management Officer call. Additionally, in June 2020, the HIV, Hepatitis, and Related Conditions Programs (HHRC) in VHA's Office of Specialty Care Services, provided information during the HIV Lead Clinicians' call and in an email to all HIV Lead Clinicians about how providers can sign up to be notified when the EPRP data have been published. As such, we are closing this recommendation as implemented.
|
| Department of Veterans Affairs | The Under Secretary for Health should disseminate data to HIV lead clinicians on the extent to which veterans who test positive for HIV are linked to care within recommended time frames. (Recommendation 2) |
VHA concurred with this recommendation and provided regular updates on its progress in implementing it. In December 2019, the HIV, Hepatitis, and Related Conditions Programs (HHRC) in VHA's Office of Specialty Care Services sent an email to HIV lead clinicians to notify them of the availably of a report that would include updated linkage to care data. They also presented the data at their virtual conference to an audience of over 300 VAMC providers. In January 2020, HHRC posted the report through its secure SharePoint site, which is accessible to all VHA providers and, according to VHA, is updated annually. As such, we are closing this recommendation as implemented.
|