Medicaid: Further Action Needed to Expedite Use of National Data for Program Oversight
Fast Facts
State-reported data help the federal government oversee the Medicaid program, which made an estimated $36.7 billion in payment errors in 2017. However, there have been longstanding concerns that those data are not sufficient for effective oversight.
To help, federal administrators established a new data repository. Nearly all states now submit data that could be used to improve oversight and program management. However, concerns persist over the completeness and comparability of state data.
We recommended federal administrators take steps to expedite collection of complete and comparable data, and draft a plan for how they will use the data.
States Reporting Data to the New Repository, the Federal Transformed Medicaid Statistical Information System (T-MSIS), as of November 2017
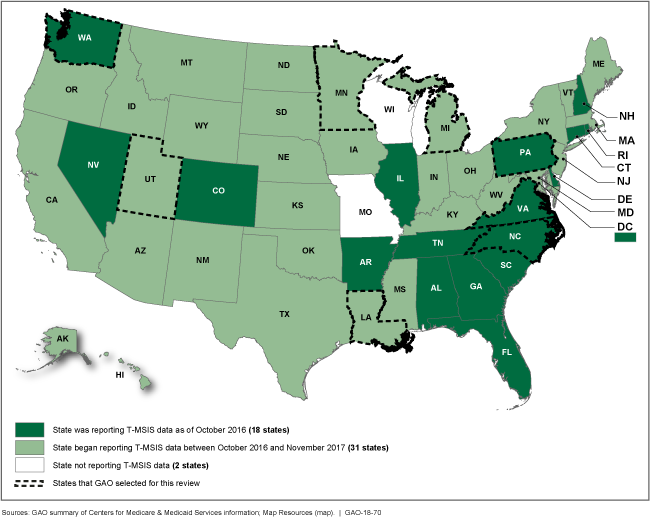
A map of the United States showing which states are participating and when they started.
Highlights
What GAO Found
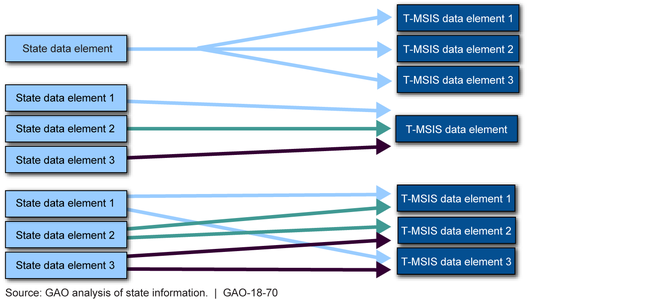
As of November 2017, 49 states had begun reporting Transformed Medicaid Statistical Information System (T-MSIS) data—a significant increase from 18 states reporting these data one year earlier. All eight states GAO reviewed identified converting their data to the T-MSIS format on an element-by-element basis as the main challenge in their reporting efforts. For some data elements, states had to expand or collapse their data to match the T-MSIS format.
Examples of Possible Relationships in Converting State Data Elements and T-MSIS Elements
With the continued implementation of T-MSIS, the Centers for Medicare & Medicaid Services (CMS) has taken an important step toward developing a reliable national repository for Medicaid data. However, data challenges have hindered states' and CMS's use of the T-MSIS data for oversight.
- None of the six selected states reporting T-MSIS data in August 2017 was reporting complete data. These states said that certain unreported elements were contingent on federal or state actions, and others were not applicable to the state's Medicaid program. States did not always specify in their documentation whether they planned to report elements in the future or when they would report complete data.
- Six of eight selected states expressed concerns about the comparability of T-MSIS data across states. Further, all states were interested in CMS facilitating information sharing among states. CMS has not compiled and shared information about states' data limitations, which would help states accurately compare their T-MSIS data to other states' T-MSIS data.
CMS has taken steps for the initial use of T-MSIS data, but does not have a plan or associated timeframes for using these data for oversight. As a result, important CMS goals for T-MSIS, such as reducing states' reporting burden and enhancing program integrity activities, are not being fully realized.
Why GAO Did This Study
GAO and others have identified insufficiencies in state-reported Medicaid data that affect CMS's ability to oversee the program effectively. Recent increases in improper payments—estimated at $36.7 billion in fiscal year 2017—exacerbate concerns about program oversight.
CMS officials identified the T-MSIS initiative, which began in 2011, as its main effort to improve Medicaid data, and cited aspects of T-MSIS aimed at improving the scope and quality of state-reported data. GAO reported in January 2017 that it is unclear when T-MSIS data will be available from all states; how CMS will ensure data quality; or how the data will be used to enhance oversight of Medicaid.
GAO was asked to review states' experiences with T-MSIS implementation and planned uses of T-MSIS data. This report examines (1) states' experiences regarding T-MSIS implementation, and (2) challenges to CMS's and states' use of T-MSIS data for oversight. GAO reviewed federal laws, guidance, and internal control standards; reviewed documents and interviewed officials from eight states, selected based on their T-MSIS reporting status, location, program expenditures, and other factors; and interviewed CMS officials, CMS contractors, and individuals involved with other states' T-MSIS efforts.
Recommendations
GAO recommends that CMS (1) improve T-MSIS's completeness and comparability to expedite its use, and (2) articulate a specific oversight plan. The Department of Health and Human Services concurred with GAO's recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services |
Priority Rec.
The Administrator of CMS, in partnership with the states, should take additional steps to expedite the use of T-MSIS data for program oversight. Such steps should include, but are not limited to, efforts to (1) obtain complete information from all states on unreported T-MSISdata elements and their plans to report applicable data elements; (2) identify and share information across states on known T-MSIS datalimitations to improve data comparability; and (3) implement mechanisms, such as the Learning Collaborative, by whichstates can collaborate on an ongoing basis to improve thecompleteness, comparability, and utility of T-MSIS data.(Recommendation 1) |
HHS concurred with this recommendation. As of March 2021, CMS has implemented several initiatives to improve the accuracy and completeness of T-MSIS data to expedite their use in Medicaid program oversight. These initiatives include: (1) Monitoring and assessing key data elements for accuracy and completeness. These efforts include providing immediate feedback to states on their monthly data submissions, and establishing and assessing data against T-MSIS priority item standards-areas of data CMS has identified as critical to program oversight. In particular, CMS has implemented an interactive web-based, operational dashboard through which it shares information on data errors identified through automated checks that provide feedback on data format and consistency. CMS also provides feedback on the extent to which data submissions meet agency standards for T-MSIS data, including standards related to completeness and accuracy. As of October 2021, CMS is assessing states' monthly data submissions against standards for 32 T-MSIS priority items. CMS also reports on its website states' progress in meeting standards for priority items. (2) Making T-MSIS data and information about the quality of these data publicly available. CMS has released T-MSIS research-ready analytic files for fiscal years 2014 through 2016, which contain data across the states. To help users understand and navigate these files, CMS introduced the Data Quality (DQ) Atlas, which presents various quality assessments of data in these files. Specifically, the DQ Atlas allows states and researchers to explore data quality by topic-such as enrollment, expenditures, and utilization-and by state. (3) Supporting collaborative learning about T-MSIS data quality. CMS obtains input from states and shares lessons learned and best practices through national webinars. CMS officials also report testing the data dashboards with states and enlisting states' assistance in developing a consolidated T-MSIS data guide. In light of these efforts, we are closing this recommendation as implemented.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should articulate a specific plan and associated time frames for using T-MSIS data for oversight. (Recommendation 2) |
HHS concurred with this recommendation. As of March 2024, CMS has addressed this recommendation by continuing to create and release additional T-MSIS data files and use the data for program research and oversight. Specifically, CMS created T-MSIS Analytic Files (TAF)-files prepared for research-which include information on Medicaid and CHIP enrollment, demographics, service utilization, and payments. CMS also prepared multiple data sets based on T-MSIS data, including data sets that inform different aspects of program oversight. For example, one data set includes metrics on Medicaid eligibility redeterminations following the COVID-19 public health emergency, while another provides information on maternal morbidity. In addition, CMS continues to use T-MSIS data to inform its oversight. For example, CMS has used T-MSIS data to: (1) report on states' participation in Money Follows the Person demonstrations under which states receive enhanced federal matching funds for health and community-based services; (2) monitor the effects of COVID-19 on Medicaid and CHIP enrollment and utilization; (3) create and publish an annual substance use disorder (SUD) data book, which includes information on the number of Medicaid beneficiaries with SUD and SUD-related services received, as well as assess the accuracy and completeness of state grantees' data regarding SUD provider types and services furnished; (4) populate certain measures in the Medicaid & CHIP Scorecard to increase public transparency about programs' administration and outcomes; and (5) develop a data clearinghouse to support business needs from different divisions of the agency. For example, CMS has used T-MSIS data to monitor whether Medicaid beneficiaries aged 20 and under received appropriate services under the Early and Periodic Screening, Diagnostic, and Treatment benefit. In light of CMS's ongoing efforts to develop and release additional T-MSIS data sets and use the data for research and oversight purposes we are closing this recommendation as implemented.
|
