Defense Health Care: Expanded Use of Quality Measures Could Enhance Oversight of Provider Performance
Fast Facts
DOD’s Military Health System allows patients to use military or civilian health care providers. We examined the measures DOD's leadership reviews to assess providers' quality of care across its health system and found that DOD:
is not using common measures across all providers;
uses measures covering a limited range of medical conditions; and
hasn’t created consistent standards and requirements related to providers' performance on the measures.
We recommended that, for all providers, DOD use common key quality measures, expand their range, and develop consistent performance standards and requirements.
Picture of the Department of Defense at the Pentagon
Highlights
What GAO Found
The National Defense Authorization Act for fiscal year 2016 (NDAA 2016) directed the Department of Defense (DOD) to align its measures of health care quality used in the Military Health System (MHS) to improve beneficiary experience and reduce variation in the quality of care. GAO reviewed the quality measures DOD identified in March 2017 in response to the NDAA 2016; DOD senior leadership tracks these measures on dashboards to gauge progress on MHS strategic goals. GAO found that DOD does not use a common set of measures on its dashboards to assess the quality of care provided by either military hospitals and clinics—known as direct care—or networks of civilian hospitals and other providers, known as purchased care. (See figure.) As a result, DOD's senior leadership has limited information on the extent to which MHS beneficiaries receive consistently high quality care across the MHS.
Figure: Number of Core Direct Care Dashboard and Purchased Care Dashboard Measures Used in the Military Health System, as of March 31, 2018
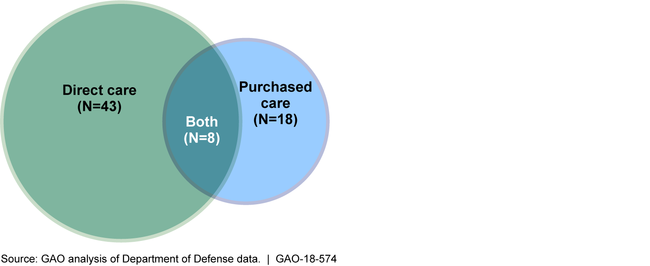
Furthermore, for both direct and purchased care, DOD uses measures on its dashboards that track a limited range of quality care areas and medical conditions compared to the measures adopted by Medicare and by private health insurers. For example, whereas civilian hospitals report to Medicare information on 11 measures of patients' self-reported experience in hospitals, Military hospitals report only 1 such measure. By using a limited range of quality measures, DOD may not detect key quality issues. Further, when selecting quality measures, the MHS does not prioritize using common measures across direct and purchased care or expanding the range of measures it uses.
GAO also found that for direct care DOD has established performance standards and corrective action requirements for military hospitals or clinics that do not meet those standards in direct care. The performance standards indicate the level of performance providers should meet on the various quality measures DOD tracks on its dashboards, and the corrective action requirements instruct providers to take steps to improve care. However, for purchased care, DOD has not established similar performance standards for individual providers. Without consistent performance standards and corrective action requirements, DOD is limited in its ability to address variation in the quality of care delivered and help ensure that its beneficiaries receive consistent high quality care across the MHS.
Why GAO Did This Study
The National Defense Authorization Act for fiscal year 2016 contains provisions for GAO to review DOD's plans to (1) improve the experience of beneficiaries who receive care through military hospitals and clinics or from civilian providers and (2) reduce variation in the quality of care.
In this report, GAO examines (1) measures DOD uses to assess the quality of direct and purchased care, and (2) the extent to which DOD has established performance standards related to the measures and corrective action requirements for providers who do not meet those standards.
GAO reviewed the measures in DOD's Core Dashboard for direct care and Purchased Care Dashboard for purchased care. It also reviewed DOD documents and reports to Congress, and interviewed MHS officials, including officials from the Army, Navy, and Air Force. GAO also compared the quality measures DOD uses to those used in Medicare and by private insurers, which have been vetted by multiple stakeholders. GAO assessed DOD's use of performance standards and corrective action requirements in the context of federal internal control standards.
Recommendations
The MHS should (1) prioritize, as appropriate, selecting quality measures common for both direct and purchased care that expand the range of quality areas covered by the measures and (2) establish consistent performance standards and corrective action requirements for direct and purchased care providers. DOD concurred with both recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Office of the Assistant Secretary of Defense (Health Affairs) | As MHS governing bodies conduct their recurring reviews of quality measures selected for MHS's Core Dashboard and Purchased Care Dashboards, the Assistant Secretary of Defense for Health Affairs should direct those bodies to prioritize, as appropriate, the selection of measures that apply to both direct and purchased care at the provider level and that expand the range of quality measure types and medical conditions that are assessed. (Recommendation 1) |
DoD concurred with this recommendation and has provided several updates since describing its plans to implement it. In May 2025 DoD provided a broad description of its expanded employment of quality of care measures applied jointly to both its direct care and purchased care providers. In June 2025 it responded to follow-up questions with more information on the specific measures in place, providing documentation of an expansion in the range of measure types in use and medical conditions assessed. We are therefore closing this recommendation as implemented.
|
| Office of the Assistant Secretary of Defense (Health Affairs) | The Assistant Secretary of Defense for Health Affairs should establish, as appropriate, performance standards related to the Purchased Care Dashboard measures that are consistent with the MHS's performance standards for direct care; ensure they are applied to individual purchased care providers; and take steps, such as amending its managed care support contracts, if necessary, to require corrective actions to be taken when providers do not meet those standards. (Recommendation 2) |
DOD concurred with this recommendation. In April 2021, DOD reported that the Defense Health Agency was in the planning phase for addressing recommendation 2 since the initiation of action was dependent upon completion of actions provided for in recommendation 1. In April 2022, DOD reported that the Defense Health Agency made changes to the next round of the TRICARE purchased care contract to establish specific clinical quality requirements with expectations for meeting consistent standards. New requirements for clinical quality monitoring at the individual level have also been incorporated into the next round of the TRICARE contract. As part of its April 2022 update, DOD reported on a set of key corrective actions with expected completion dates to address this recommendation; for example, DOD expects to establish consistent performance standards for measures identified for both direct care and purchased care by September 2023. In December 2023, DOD reported that next generation of contracts were awarded but were currently in protest status. DOD provided a new estimated completion date of December 31, 2025, and reiterated this estimated completion date in March 2025. We will update this recommendation as DOD provides progress updates on the implementation of these plans.
|
