Medicare Fee-For-Service: Information on the First Year of Nationwide Reduced Payment Rates for Durable Medical Equipment
Fast Facts
Historically, Medicare used a standard set of rates to pay for certain durable medical equipment (i.e., walkers and oxygen) for its beneficiaries. Due to concerns that it was paying higher than market rates, Medicare began a competitive bidding program for some of these items in designated areas in 2011. In 2016, information from this program was used to reduce rates in the rest of the country.
We found that the number of suppliers who sold these items decreased—continuing a long-term trend—but that available information indicates that beneficiaries were able to get needed items.
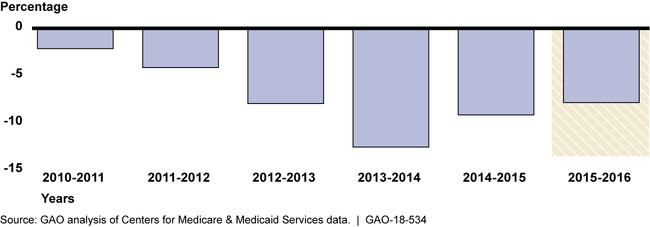
Percentage Decrease in the Number of Suppliers Furnishing Durable Medical Equipment Items

Bar graph showing changes in the number of durable medical equipment suppliers.
Highlights
What GAO Found
The Centers for Medicare & Medicaid Services (CMS) implemented a competitive bidding program (CBP) for certain durable medical equipment (DME), such as wheelchairs and oxygen, in 2011 that is currently operating in 130 designated U.S. areas. On January 1, 2016, CMS used information from the CBP to start adjusting Medicare fee-for-service payment rates for certain DME throughout the country in areas that had previously not been subject to the CBP (known as non-bid areas). For the first year adjusted rates were in effect in non-bid areas, GAO found:
Reductions in payment rates were generally significant but varied by category of DME item. The unweighted average reduction in payment rates for the five rate-adjusted DME items with the highest expenditures in 2016 within each DME category was 46 percent.
Changes in the number of suppliers furnishing rate-adjusted items were generally consistent with the years before adjusted rates went into effect. GAO found that the number of suppliers furnishing rate-adjusted items in non-bid areas in 2016 decreased 8 percent compared to 2015.
GAO's review of Medicare claims data found that beneficiary utilization of rate-adjusted items in non-bid areas in 2016 showed little change compared to 2015. GAO also found that CMS's activities to monitor beneficiary access, including changes in health outcomes, showed little change between 2015 and 2016.
Year-to-Year Percentage Decrease in the Number of Suppliers Furnishing Rate-Adjusted Durable Medical Equipment Items in Non-Bid Areas, 2010 to 2016
GAO interviewed several stakeholder groups that reported anecdotal examples of specific beneficiary access concerns they attributed to the rate adjustments, but stakeholders could not provide evidence to substantiate that the access issues were widespread. GAO's findings are consistent with CMS's monitoring results, which indicate that there were no widespread effects on beneficiary access in the year after the adjusted rates went into effect. However, some effects may take longer to appear, underscoring the importance of CMS's continued monitoring activities.
The Department of Health and Human Services provided technical comments on a draft of this report, which GAO incorporated as appropriate.
Why GAO Did This Study
To achieve Medicare DME savings, Congress required CMS to implement a CBP in certain geographic areas for certain DME items. Beginning in 2011, CMS began implementing the CBP in several phases. The agency estimates that the CBP will save the Medicare program $19.7 billion between 2013 and 2022.The Patient Protection and Affordable Care Act required CMS to use CBP information to adjust fee-for-service payment rates for certain DME items in non-bid areas. On January 1, 2016, adjusted rates for 393 items went into effect in non-bid areas. CMS estimated these adjustments will save the Medicare program about $3.6 billion between fiscal years 2016 and 2020.
GAO was asked to review the potential effects of reduced payment rates for DME in non-bid areas. In this report, GAO examines (1) payment rate reductions and any changes in the number of suppliers; (2) any changes in the utilization of rate-adjusted items; and (3) available evidence related to potential changes in beneficiaries' access to rate-adjusted items.
GAO compared non-adjusted 2015 fee-for-service payment rates to adjusted 2016 and 2017 rates and reviewed Medicare claims data from 2010 through 2016. GAO also reviewed CMS's monitoring activities and interviewed CMS officials. In addition, GAO interviewed select beneficiary advocacy groups and DME industry trade organizations.
For more information, contact A. Nicole Clowers at (202) 512-7114 or clowersa@gao.gov.
