Medicare Advantage: CMS Should Use Data on Disenrollment and Beneficiary Health Status to Strengthen Oversight
Fast Facts
Under the Medicare Advantage program, private insurance companies contract with the Centers for Medicare & Medicaid Services (CMS) to offer health plans that cover all services required by Medicare.
We found some contracts in which people in poor health were much more likely than others to voluntarily leave the contracts' health plans. These contracts generally had lower quality scores, and their enrollees often cited problems getting access to care.
We recommended that CMS consider using data on the health status of people who leave Medicare Advantage contracts, and the reasons they give for leaving to help improve oversight of the program.
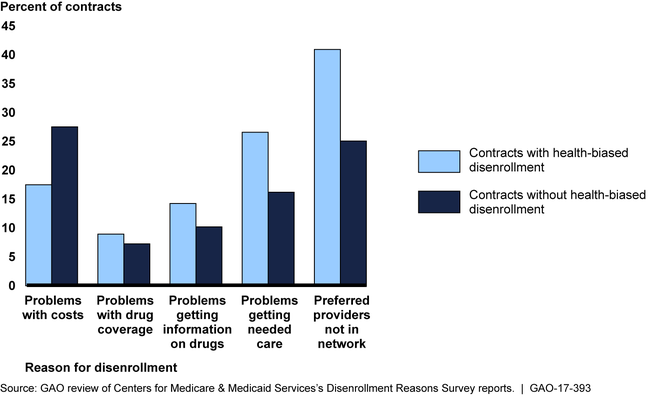
Disenrollment Reasons Survey Responses for the 126 Medicare Advantage Contracts with Relatively High Disenrollment, 2014
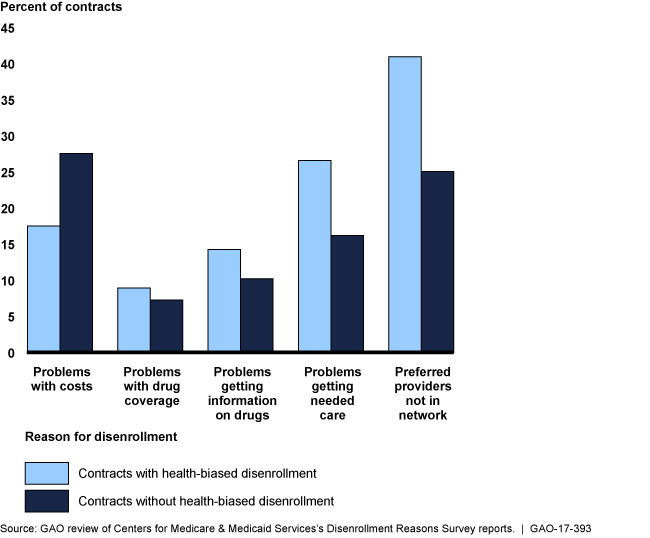
Bar chart showing reasons why healthier and less-healthy people left contracts.
Highlights
What GAO Found
Under the Medicare Advantage (MA) program, the Centers for Medicare & Medicaid Services (CMS) contracts with private entities to offer coverage for Medicare beneficiaries. GAO examined 126 contracts with higher disenrollment rates—above the median rate of 10.6 percent in 2014—and found 35 contracts with health-biased disenrollment. In these contracts, beneficiaries in poor health were substantially more likely (on average, 47 percent more likely) to disenroll relative to beneficiaries in better health. Such disparities in contract disenrollment by health status may indicate that the needs of beneficiaries, particularly those in poor health, may not be adequately met.
GAO found that beneficiaries who left the 35 contracts with health-biased disenrollment tended to report leaving for reasons related to preferred providers and access to care. In contrast, beneficiaries who left the 91 contracts without health-biased disenrollment tended to report that they left their contracts for reasons related to the cost of care.
Disenrollment Reasons Survey Responses for the 126 Medicare Advantage Contracts with Relatively High Disenrollment, 2014
CMS does not use available data to examine data on disenrollment by health status as part of its ongoing oversight; thus, CMS may fail to identify problems in MA contract performance, which poses a risk as contracts are prohibited from limiting coverage based on health status. CMS's oversight is inconsistent with internal control standards.
Why GAO Did This Study
In 2016, over 30 percent of Medicare beneficiaries were enrolled in the MA program. Each year beneficiaries have an opportunity to join or leave their MA plan.
GAO was asked to review MA disenrollment by health status and CMS oversight. This report examines, among other issues, (1) the extent of any health-biased disenrollment, (2) beneficiaries' reasons for leaving contracts with and without health biased disenrollment, and (3) how, if at all, CMS identifies contracts with health-biased disenrollment, for routine oversight purposes.
GAO analyzed 2014 disenrollment rates for the 252 MA contracts that had a sufficient number of disenrollees and met other criteria. For the 126 contracts with disenrollment rates above the median rate, GAO used beneficiaries' projected health care costs to identify those in poor health and better health. GAO examined data from CMS's Disenrollment Reasons Survey to learn why beneficiaries reported leaving the 126 contracts with relatively high disenrollment rates. GAO also interviewed CMS officials and compared their oversight to federal standards for internal control.
Recommendations
To strengthen its oversight of MA contracts, CMS should examine data on disenrollment by health status and the reasons beneficiaries disenroll. HHS concurred with GAO's recommendation.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | To strengthen CMS's oversight of MA contracts, the Administrator of CMS should review data on disenrollment by health status and the reasons beneficiaries disenroll as part of the agency's routine monitoring efforts. |
In response to our recommendation in 2017, CMS conducted an analysis of Medicare Advantage contracts with a large number of enrollees in poor health. Specifically, CMS examined contracts' disenrollment rates, Disenrollment Reasons Survey scores, and Star Ratings to identify outlier contracts ( e.g., contracts with a high percentage of disenrollees in poor health or high responses for a particular reason for disenrollment). CMS stated that program staff will work with outlier contracts to address issues and if necessary, will determine if compliance actions are appropriate. CMS stated that it will conduct this analysis on an annual basis.
|
