Why are Urban Hospitals Closing and What Happens After They Do?
In recent years, more hospitals have closed than opened in urban areas. Hospital closures like these can affect patients’ ability to receive the right care at the right place at the right time.
Why are urban hospitals closing and what happens after they do? Today’s WatchBlog post looks at our new report about this issue.
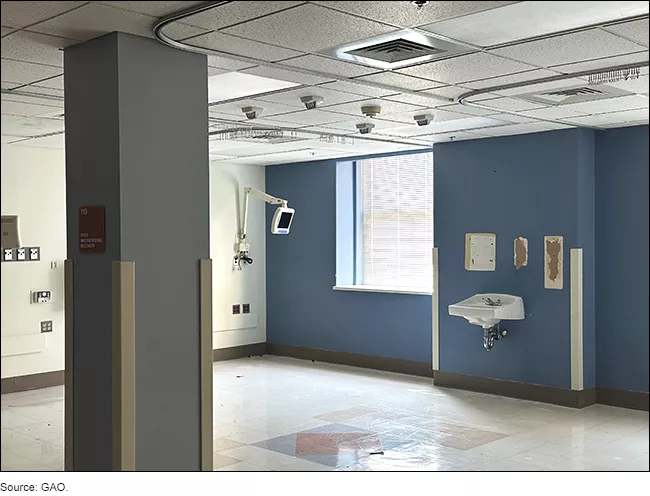
Empty Patient Room After Hospital Closure
Image
Why are urban hospitals closing?
About 80% of the U.S. population lives in urban areas. Urban hospitals make up about half of U.S. hospitals and provide essential health care to both urban and nearby rural communities, including complex surgeries and critical emergency care. Despite their importance, more urban hospitals have closed than opened over the last 5 years.
Why is this happening? For our new report, we looked at five recent urban hospital closures across the country. All five of these hospitals struggled financially prior to closure. And representatives from these hospitals told us that their financial condition was a key factor that contributed to their closure. For example, one hospital had filed for bankruptcy three times within the 5 years leading up to its eventual closure.
But financial decline wasn’t the only factor driving these closures. In all the cases we looked at, a combination of other contributing issues led to eventual closure, including:
- Aging facilities requiring costly repairs or upgrades.
- Low or declining patient volumes due to reduced services, lack of employed physicians, and competition from other hospitals.
- Poor management practices, such as incorrect billing or lack of payments for services.
- Challenges operating an independent hospital without the support of a multihospital system.
- Separate ownership interests, where one entity owns the hospital business and another the real estate.
Examples of Hospital Infrastructure in Disrepair, 22 Months After Closure
Image

What happens after the 5 urban hospitals we looked at closed?
Even in areas with multiple hospitals, hospital closures can negatively impact access to care. This is especially true when the closure reduces access to emergency and specialty services. For example, some of the closed hospitals we looked at provided time-sensitive, lifesaving services—such as obstetrics, heart surgery, or emergency care. After they closed, patients often had to travel farther, and nearby hospitals became overcrowded.
What happened to the five urban hospitals after they closed? Two converted into outpatient facilities. The other three shut down completely, ending all health services.
In some communities, local efforts helped fill the gaps. For example, access shifted to different settings or providers in communities where the two hospitals converted:
- One closed hospital became a standalone emergency department.
- Another closed hospital introduced urgent care to replace its emergency department.
- Nearby hospitals also increased their capacity by adding more beds or services.
In some communities where hospitals closed completely, there was a reduction in available health care services. Community members also told us that they received limited advance notice, in some cases leaving residents with little time to prepare for the closures. In communities already grappling with access challenges, closures may have exacerbated long-standing issues with getting needed health care.
With that said, each community is different. And the impact of these closures may vary. Most of the hospitals we looked at were considered “safety-net” hospitals and served low-income and racially diverse inner-city neighborhoods. Many residents in these communities already face barriers accessing care. For example, some residents lacked adequate transportation to reach alternative hospitals or clinics or were not aware of other providers, further complicating their ability to access necessary and timely care.
You can learn more about hospital closures and their impacts by checking out our new report. These challenges are not unique to urban hospitals. Many rural hospitals face similar issues. Check out our 2023 blog to learn more.
- GAO’s fact-based, nonpartisan information helps Congress and federal agencies improve government. The WatchBlog lets us contextualize GAO’s work a little more for the public. Check out more of our posts at GAO.gov/blog.
- Got a comment, question? Email us at blog@gao.gov.
GAO Contacts
Related Products

GAO's mission is to provide Congress with fact-based, nonpartisan information that can help improve federal government performance and ensure accountability for the benefit of the American people. GAO launched its WatchBlog in January, 2014, as part of its continuing effort to reach its audiences—Congress and the American people—where they are currently looking for information.
The blog format allows GAO to provide a little more context about its work than it can offer on its other social media platforms. Posts will tie GAO work to current events and the news; show how GAO’s work is affecting agencies or legislation; highlight reports, testimonies, and issue areas where GAO does work; and provide information about GAO itself, among other things.
Please send any feedback on GAO's WatchBlog to blog@gao.gov.




