Medicare Advantage: Limited Progress Made to Validate Encounter Data Used to Ensure Proper Payments
Fast Facts
Medicare Advantage organizations—which offer a private health plan alternative to traditional Medicare—were paid about $170 billion by the federal government and served nearly one-third of all Medicare beneficiaries in 2015. To help ensure appropriate payments, the Centers for Medicare & Medicaid Services collects data on the care and health status of Medicare Advantage enrollees.
We previously reported that CMS had not fully validated these data for completeness and accuracy. In this review, we found that CMS has conducted some, but not all, remaining validation steps. We maintain that complete validation is key to ensuring data quality.
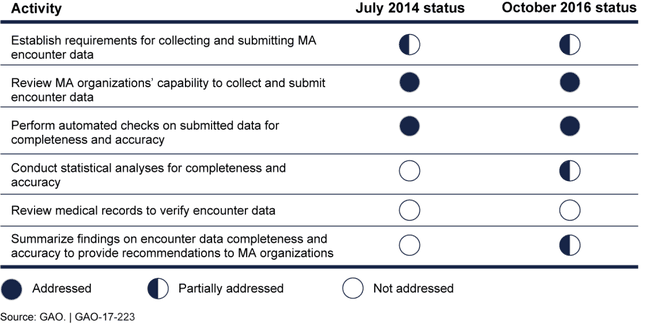
Change in Status of the Centers for Medicare & Medicaid Services' Actions to Validate Medicare Advantage (MA) Encounter Data, from July 2014 to October 2016
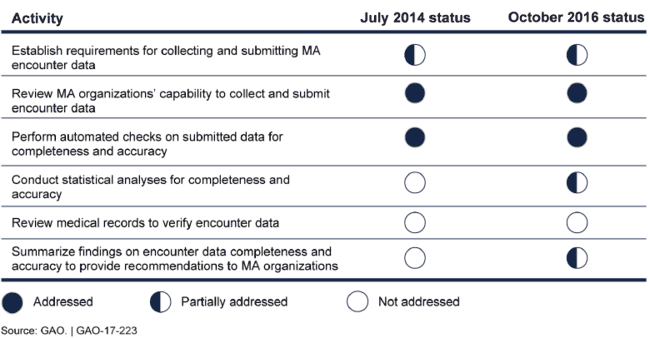
Table showing 6 activities: 2 complete, 3 partly met as of October 2016, and 1 not addressed.
Highlights
What GAO Found
Since GAO issued its July 2014 report, the Centers for Medicare & Medicaid Services (CMS) within the Department of Health and Human Services (HHS) has made limited progress to validate the completeness and accuracy of Medicare Advantage (MA) encounter data. CMS collects encounter data—detailed information about the care and health status of MA enrollees—to determine payments to MA organizations (MAO). These entities received approximately $170 billion to provide coverage to nearly one-third of all Medicare beneficiaries in 2015. The agency uses a risk adjustment process to account for differences in enrollees' expected health care costs relative to an average beneficiary. Without complete and accurate encounter data, CMS cannot appropriately risk adjust MAO payments. CMS has begun compiling basic statistics on the volume and consistency of data submissions and preparing automated summary reports for MAOs indicating diagnosis information used for risk adjustment. However, CMS has yet to undertake activities that fully address encounter data accuracy, such as reviewing medical records. (See figure.) Furthermore, some health insurance and provider trade associations GAO interviewed voiced concerns about CMS's ability to properly identify diagnoses used for risk adjustment. CMS officials noted that they are working with MAOs to refine how the methodology used to obtain diagnoses data is applied. To the extent that CMS is making payments based on data that have not been fully validated for completeness and accuracy, the soundness of billions of dollars in Medicare expenditures remains unsubstantiated. Given the agency's limited progress, GAO continues to believe that CMS should implement GAO's July 2014 recommendation that CMS fully assess data quality before use.
Change in Status of the Centers for Medicare & Medicaid Services' Actions to Validate Medicare Advantage (MA) Encounter Data, from July 2014 to October 2016
Since the July 2014 report, CMS has made progress in developing plans to use MA encounter data for risk adjustment, but has not specified plans and time frames for most other purposes, such as conducting program evaluations and supporting public health initiatives. CMS began phasing in patient diagnosis information from encounter data in its risk adjustment process in 2015 and intends to rely completely on those data by 2020. Because it has primarily focused on collecting comprehensive encounter information for risk adjustment purposes—which is key to ensuring proper payments—CMS officials told GAO that the agency has largely deferred planning for additional uses of the data. Some stakeholder organizations have objected to the risk adjustment transition time frame, asserting that it does not allow sufficient time for a successful transition. According to CMS, the multiyear transition time frame is reasonable. Some stakeholders also were concerned that releasing data to external entities could compromise the confidentiality of proprietary information, such as payments to providers. CMS officials said that they intend to use data protections similar to those used with other Medicare data. In the absence of planning for all of the authorized uses, the agency cannot be assured that the amount and types of data being collected are necessary and sufficient for specific purposes. Given the agency's limited progress, GAO continues to believe that CMS should implement GAO's July 2014 recommendation that CMS fully develop plans for the additional uses of encounter data.
Why GAO Did This Study
CMS collects MA encounter data to help ensure the proper use of federal funds by improving risk adjustment in the MA program—the private health plan alternative to traditional Medicare—and for other potential purposes. CMS's ability to make proper payments depends on the completeness and accuracy of MA encounter data. In July 2014, GAO reported that CMS had taken some, but not all, appropriate actions to validate the completeness and accuracy of encounter data and had not fully developed plans for using them.
GAO was asked to provide an update on its July 2014 findings. In this report, GAO identifies (1) steps CMS has taken to validate MA encounter data, and (2) CMS's plans and time frames for using MA encounter data—as well as stakeholder perspectives on these steps and plans.
To do this work, GAO compared CMS activities with the agency's protocol for validating Medicaid encounter data—comparable data collected and submitted by entities similar to MAOs—and federal internal control standards. In addition, GAO reviewed relevant agency documents and interviewed CMS officials on MA encounter data collection and reporting. GAO also reviewed comments in response to CMS's 2014 proposed rule and reports from stakeholder organizations. GAO also interviewed a non-generalizable selection of 11 stakeholders including health insurance and provider trade associations and research organizations. HHS provided technical comments on this report that were incorporated as appropriate.
For more information, contact James Cosgrove at (202) 512-7114 or cosgrovej@gao.gov.
