Medicaid: CMS Needs Better Data to Monitor the Provision of and Spending on Personal Care Services
Fast Facts
Millions of Medicaid beneficiaries rely on personal care services for help with daily tasks like bathing and eating. However, these types of services are at high risk for fraud and abuse—e.g., services that were paid for but never provided.
We found that the Centers for Medicare & Medicaid Services needs better data to oversee these personal care services. In 2012, for example, $4.9 billion worth of these claims did not identify the person who provided the service.
We recommended that CMS issue guidance to states for reporting key data, ensure that data meet requirements, and develop plans to use this data for oversight.
Percentage of 2012 Medicaid Claims and Encounters for Personal Care Services in 35 States That Had Complete Information on Payment, Provider Information, and the Quantity of Services Provided
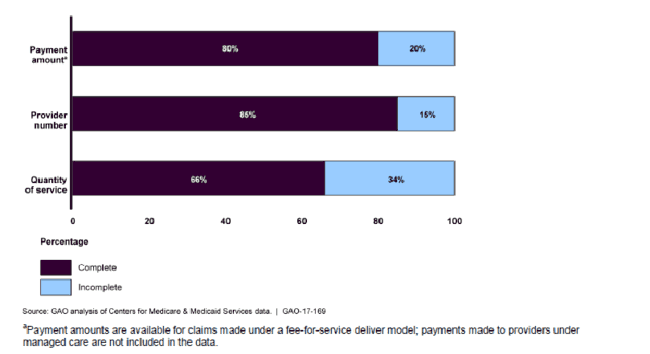
Bar graph showing the completeness of Medicaid claims data for personal care services in 2012.
Highlights
What GAO Found
Two data systems managed by the Centers for Medicare & Medicaid Services (CMS)—the federal agency that oversees Medicaid—collect information from states on the provision of and spending on personal care services:
- The Medicaid Statistical Information System (MSIS) collects detailed information from provider claims on services rendered to individual Medicaid beneficiaries and state payments for these services.
- The Medicaid Budget and Expenditure System (MBES) collects states' total aggregate Medicaid expenditures across 80 broad service categories.
Information from these two CMS data systems can be used in the aggregate to describe broadly the provision of and spending on Medicaid personal care services. For example, MBES data show that total fee-for-service spending on these services was at least $15 billion in 2015—up $2.3 billion from 2012.
However, the usefulness of the data collected from these two systems for CMS oversight is limited because of data gaps and errors. To provide effective oversight, including decision making, external reporting, and monitoring program operations, CMS needs timely, relevant and reliable data on personal care services rendered and the amount paid. GAO found that the data collected did not always meet these standards. For example:
- MSIS data were not timely, complete, or consistent. The most recent data available at the time of GAO's audit were for 2012 and only included data for 35 states. Further, 15 percent of claims lacked provider identification numbers, over 400 different procedure codes were used to identify the services, and the quantity and time periods varied widely. Without good data, CMS is unable to effectively monitor who is providing personal care services or the type, amount, and dates of services. CMS may also face challenges determining whether beneficiaries were eligible for services and assessing the reasonableness of the amount of services claimed.
- MBES data were not always accurate or complete. From 2012 through 2015, GAO found that 17 percent of expenditure lines were not reported correctly. Nearly two-thirds of these errors were due to states not separately identifying personal care services expenditures, as required by CMS. Inaccurate and incomplete reporting limits CMS's ability to ensure federal matching funds are provided consistent with states' approved programs.
CMS is developing a new Medicaid claims system to replace MSIS and recently established a new office to support CMS's use of Medicaid data for program management and monitoring. However, CMS has not issued guidance related to reporting of personal care services that addresses the gaps GAO identified, or developed plans to use the data for oversight purposes. Without improved data and plans for how it can be used for oversight, CMS could continue to lack critical information on personal care service expenditures.
HHS agreed with two of GAO's recommendations to ensure state compliance with reporting requirements and develop plans to use the data. HHS neither agreed nor disagreed with two others.
Why GAO Did This Study
A growing share of long-term care spending under Medicaid, a joint federal-state health care program, is for services provided in home and community settings. Medicaid spending on these services—about $80 billion in 2014—now exceeds spending on institutional long term care. Personal care services are key components of long-term, in-home care, providing assistance with basic activities, such as bathing, dressing, and toileting, to millions of individuals seeking to retain their independence and to age in place. However, these services are also at high risk for improper payments, including fraud.
Given the expected increase in the demand for and spending on personal care services and risk of improper payments, GAO was asked to examine available data on personal care services and CMS's use of the data. This report: (1) describes the CMS systems that collect data on personal care services and what the data reveal, and (2) examines the extent to which data from these systems can be used for oversight. GAO reviewed information from two CMS data systems, reviewed relevant federal guidance and documents, and interviewed officials and researchers.
Recommendations
GAO recommends that CMS improve personal care services data by: establishing standard reporting guidance for key data; ensuring linkage between data on the provision of services and reported expenditures; ensuring state compliance with reporting requirements; and developing plans to use data for oversight.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | To improve the collection of complete and consistent personal care services data and better ensure CMS can effectively monitor the states' provision of and spending on Medicaid personal care services, CMS should establish standard reporting guidance for personal care services collected through Transformed-MSIS (T-MSIS) to ensure that key data reported by states, such as procedure codes, provider identification numbers, units of service, and dates of service, are complete and consistent. |
The Centers for Medicare & Medicaid Services (CMS) concurred with GAO's recommendation, and in February 2018, the agency distributed guidance to address the challenges states have shown in reporting complete and consistent claims data on Medicaid personal care services. The guidance clarifies that states should include key data elements in each claim for Medicaid personal care services reported through T-MSIS, the agency's new claims reporting system, including provider identification numbers, dates of service, and quantities of services provided. The guidance also specifies that a national coding system should be used to consistently identify the services provided to beneficiaries. By issuing standard reporting guidance, CMS will have better data needed to oversee Medicaid personal care services.
|
| Centers for Medicare & Medicaid Services | To improve the collection of complete and consistent personal care services data and better ensure CMS can effectively monitor the states' provision of and spending on Medicaid personal care services, CMS should better ensure, for all types of personal care services programs, that data on provision of personal care services and other home-and community-based services (HCBS) collected through T-MSIS claims can be specifically linked to the expenditure lines on the CMS-64 that correspond with those particular types of HCBS services. |
The Centers for Medicare & Medicaid Services (CMS) concurred with this recommendation, and in February 2018, the agency distributed guidance to states on reporting claims for Medicaid personal care services in T-MSIS, the agency's new claims reporting system. CMS included as a required data element a field to indicate the corresponding expenditure reporting line on the CMS-64. The guidance also specified that each claims must indicate the type of service as personal care services. These two reporting requirements, taken together, will allow CMS to identify and compare total personal care service claims for each program type within a state with the total corresponding aggregate expenditures reported in the CMS-64. By linking the two data systems, CMS will be better able to validate states' reported expenditures on personal care services.
|
| Centers for Medicare & Medicaid Services | To improve the collection of complete and consistent personal care services data and better ensure CMS can effectively monitor the states' provision of and spending on Medicaid personal care services, CMS should better ensure that personal care services data collected from states through T-MSIS and MBES comply with CMS reporting requirements. |
The Centers for Medicare & Medicaid Services (CMS) concurs with GAO's recommendation. In December 2017, CMS cited ongoing efforts related to claims data submitted by states through T-MSIS, CMS's new claims reporting system. Efforts included validation checks of personal care service claims to ensure that key data are not missing or incorrect. In addition, CMS issued technical guidance in February 2018 directing states to fill out claims for personal care services accurately and completely, including the type, amount, and dates of services. In contrast, as of December 2025, CMS has not reported implementing systems to identify inaccurate state reporting of personal care expenditures through CMS's expenditure reporting system, Medicaid Budget and Expenditure System (MBES). Complete implementation of the recommended action will better ensure state reporting of claims and expenditures is accurate and will allow CMS to effectively perform key management functions.
|
| Centers for Medicare & Medicaid Services | To improve the collection of complete and consistent personal care services data and better ensure CMS can effectively monitor the states' provision of and spending on Medicaid personal care services, CMS should develop plans for analyzing and using personal care services data for program management and oversight. |
The Centers for Medicare & Medicaid Services (CMS) concurred with this recommendation, and in January 2022, CMS reported that the agency, working with a contractor, had implemented a plan for analyzing and using personal care services data as GAO recommended in January 2017. Specifically, CMS and its contractor developed and executed a workplan to analyze how the implementation of Electronic Visit Verification affected the utilization of personal care services across the states, and then used this information to assist targeted states. By developing and implementing a plan for analyzing and using personal care services data, CMS has improved the information available for oversight and management of personal care services.
|
