VA Real Property: Leasing Can Provide Flexibility to Meet Needs but VA Should Demonstrate the Benefits
Highlights
What GAO Found
The Department of Veterans Affairs (VA) leases major medical facilities to benefit from shorter time frames to open a facility and to attain flexibility to relocate. These factors may help VA to meet its needs, such as improving facility compliance with standards and increasing veterans' access to care and services. Unlike owned facilities that can be difficult to dispose of, VA must vacate leased facilities at the end of the lease term, which can allow VA to relocate to space better aligned with its needs. Leases executed under a delegation of authority from the General Services Administration (GSA) can be obligated on an annual basis, whereas owned facilities require full upfront funding that can be difficult to obtain. VA cited flexibility to move as a justification in all 51 of its proposals for these leases since 2015. VA does not, however, assess and provide information to decision makers on how it has benefited from this flexibility. Without transparency on these benefits, VA and congressional decision makers may lack information to understand the need for these leases. GAO and the Office of Management and Budget have reported on the importance of assessing the results of capital decisions in making future decisions.
VA's cost-estimating procedures for major medical facility leases generally align with GAO's 12 cost-estimating best practice steps and recent changes in VA's approach may improve the quality of VA's estimates. GAO's review of cost data for these leases since 2006 found that actual costs often varied more than 15 percent above or below the estimates included in their proposals, often due to project design changes. In 2016, VA introduced a design guide for leased medical facilities that delineates VA and federal requirements, such as security and sustainability standards, that may reduce the risk of project, and thus cost, changes from those included in proposals. VA also initiated a lessons-learned effort to evaluate the factors that contribute to differences between actual lease costs and those included in proposals. The success of these steps will depend on how quickly and effectively VA implements them.
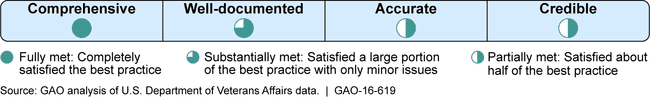
Extent to which VA's Lease Cost-Estimating Procedures Align with Best Practices
VA has made progress meeting GSA's requirements to obtain needed delegations of authority to pursue VA leases by expanding training, implementing a management review process, and working more closely with GSA. According to GSA, VA's requests for delegation of authority now regularly include required documentation, such as justifications for paying above market lease rates. As a result, VA has received delegations of authority in about 21 days, down from 58 days when VA first started to apply for delegations in July 2014. However, it is too early to assess the effectiveness of these steps with VA's prospectus-level leases, executed under GSA's delegated authority, that exceed $2.85 million in average annual rent. These leases require authorization from GSA's authorizing committees and can be more difficult to align with GSA's requirements.
Why GAO Did This Study
VA operates the largest health care network in the United States, with over 2,700 health care sites, including hospitals and outpatient facilities. However, many facilities are outdated, and VA estimates that its capital needs will require up to $63 billion over the next 10 years. In recent years, VA has increasingly leased its facilities, including major medical facilities. These facilities can exceed 200,000 square feet; provide services to veterans such as mental health and other clinical care; are generally built by private developers to meet VA and federal design requirements; and have average annual rent rates in excess of $1 million. VA must submit proposals to Congress and receive authorizations for major medical facility leases.
GAO was asked to review VA's leasing program. This report examines: (1) the factors that account for VA's decisions to lease major medical facilities; (2) the extent to which VA's cost-estimating process for leasing these facilities reflects best practices; and (3) steps VA has taken to align its lease process to GSA requirements for delegated leasing authority. GAO analyzed agency documents, VA data on major medical facility leases and lease delegation requests to GSA, compared VA's cost-estimating procedures to best practices in GAO's Cost Guide , and interviewed VA and GSA officials.
Recommendations
GAO recommends that VA assess the benefits of major medical facility leasing and use the information in VA's annual capital plans. VA concurred with GAO's recommendation, and GAO incorporated VA's technical comments as appropriate.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Department of Veterans Affairs | To enhance transparency and allow for more informed decision making related to VA's major medical facility leases, the Secretary of Veterans Affairs should annually assess how VA has benefited from flexibilities afforded by leasing its major medical facilities and use information from these assessments in its annual capital plans. |
The Department of Veterans Affairs (VA) operates the largest health care network in the United States through the Veterans Health Administration, with over 2,700 health care sites, including hospitals and outpatient facilities. In recent years, VA has increasingly leased its facilities, including major medical facilities, which have an average annual rent in excess of $1 million. In 2016, GAO reported that VA leases major medical facilities to benefit from shorter time frames to open a facility and to attain flexibility to relocate. These factors may have helped VA to meet its needs, such as improving facility compliance with standards and increasing veterans' access to care and services. VA cited flexibility to relocate in all 51 of its justifications for major medical facility leases submitted to Congress from fiscal year 2015 to fiscal year 2017. Unlike owned facilities that can be difficult to dispose of, VA must vacate leased facilities at the end of the lease term, which can allow VA to relocate to space better aligned with its needs. VA justifies leasing its major medical facilities to its department leadership and congressional decision makers based on the flexibility that leasing offers compared to other alternatives. However, VA neither provided these stakeholders with information on the extent to which it had benefited from that flexibility, nor regularly assessed information that would have helped it do so. In particular, GAO found that while VA regularly cited future "flexibility," as a justification for the leases included in its annual capital plans, the benefits that VA had experienced from this flexibility with major medical facility leases were not presented to VA stakeholders responsible for selecting projects to present to Congress or to congressional decision makers. Without transparency on these benefits, VA and congressional decision makers may lack information to understand the need for these leases. GAO and the Office of Management and Budget have reported on the importance of assessing the results of capital decisions in making future decisions. Therefore, GAO recommended that VA assess the benefits of leading major medical facilities and use the information in VA's annual capital plans. In 2018, GAO confirmed that VA had assessed the benefits of major medical facility leasing and, based on its assessment, included information explaining the benefits associated with the flexibility of leasing in its fiscal year 2018 capital plan. VA also committed to including such information in future annual capital plans. This information will provide greater transparency VA and congressional decision makers, as well as taxpayers, regarding the need and how best to pay for VA's major medical facilities.
|
